THE HUMAN GUT MICROBIOME IN HEALTH AND DISEASE
Matthew J. Bull, BSc, PhD and Nigel T. Plummer, PhD, Integrative Medicine (Encinitas). 2014 Dec; 13(6): 17–22.
Ronald Peters MD Commentary
We humans are very good at upsetting the balance of Nature. The ecology around us is polluted with chemicals, plastics and more leading to 70% loss of species and major damage to Mother Earth. We also disturb the ecology within us with the refined, polluted and mineral depleted foods that we eat. And, we create high levels of stress by activating our Fight/Flight Sympathtic Nervous System, which is designed to help us run from danger, by sitting on the couch and worrying about what could go wrong next month. Unlike our distant ancestors, health is no longer a natural part of living. We need to educate ourselves to protect our health and the health of the beautiful planet we live on.
ABSTRACT
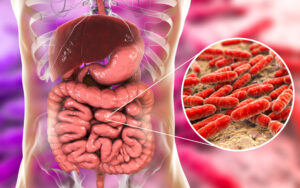 The bacterial cells harbored within the human gastrointestinal tract (GIT) outnumber the host’s cells by a factor of 10 and the genes encoded by the bacteria resident within the GIT outnumber their host’s genes by more than 100 times. These human digestive-tract associated microbes are referred to as the gut microbiome. The human gut microbiome and its role in both health and disease has been the subject of extensive research, establishing its involvement in human metabolism, nutrition, physiology, and immune function. Imbalance of the normal gut microbiota have been linked with gastrointestinal conditions such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS), and wider systemic manifestations of disease such as obesity, type 2 diabetes, and atopy (allergy). In the first part of this review, we evaluate our evolving knowledge of the development, complexity, and functionality of the healthy gut microbiota, and the ways in which the microbial community is perturbed in dysbiotic disease states; the second part of this review covers the role of interventions that have been shown to modulate and stabilize the gut microbiota and also to restore it to its healthy composition from the dysbiotic states seen in IBS, IBD, obesity, type 2 diabetes, and atopy.
The bacterial cells harbored within the human gastrointestinal tract (GIT) outnumber the host’s cells by a factor of 10 and the genes encoded by the bacteria resident within the GIT outnumber their host’s genes by more than 100 times. These human digestive-tract associated microbes are referred to as the gut microbiome. The human gut microbiome and its role in both health and disease has been the subject of extensive research, establishing its involvement in human metabolism, nutrition, physiology, and immune function. Imbalance of the normal gut microbiota have been linked with gastrointestinal conditions such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS), and wider systemic manifestations of disease such as obesity, type 2 diabetes, and atopy (allergy). In the first part of this review, we evaluate our evolving knowledge of the development, complexity, and functionality of the healthy gut microbiota, and the ways in which the microbial community is perturbed in dysbiotic disease states; the second part of this review covers the role of interventions that have been shown to modulate and stabilize the gut microbiota and also to restore it to its healthy composition from the dysbiotic states seen in IBS, IBD, obesity, type 2 diabetes, and atopy.
Microbiota in a Healthy Gut
The gut microbiota are mainly composed of strict anaerobes, which outnumber the facultative anaerobes— organisms able to grow both aerobically and anaerobically— and the aerobes by up to 100-fold.1 Although the presence of more than 50 bacterial phyla has been detected in the human gut to date,2 the microbiota are dominated by only 2 phyla: the Bacteroidetes and the Firmicutes. Estimates of the number of bacterial species present in the human gut vary widely among studies, but it is generally accepted that individuals harbor more than 1000 microbial, species-level phylotypes.3–5
Development and Composition
Microbial colonization of the human gut begins at birth. The infant’s intestines are believed to be sterile or contain a very low level of microbes at birth,6 but the GIT is quickly colonized during and after delivery. As a neonate passes through the birth canal, he or she is exposed to the microbial population of the mother’s vagina. This process influences the development of an infant’s intestinal microbiota, which show similarities to the vaginal microbiota of his or her mother. Infants who were delivered through cesarean section showed reduced microbial numbers in the gut at 1 month when compared with those who were delivered vaginally, although these differences do not remain detectable at 6 months of age.7
During the first year of life, the composition of the gut microbiota is relatively simple and shows wide interindividual variations.8 It is believed that the initial gut colonization is instrumental in shaping the composition of the adult’s gut microbiota. This fact was demonstrated by Ley et al,9 who showed that the gut microbiota of their study’s mice were closely related to that of their mothers, implicating kinship as a factor in the determination of the composition of the gut microbiota.
The infant’s gut microbiota undergo a succession of changes that are correlated with a shift in feeding mode from breast- or formula-feeding to weaning and the introduction of solid food.8 Despite the relative similarities of the gut microbiota in mothers and their offspring, microbial succession in the GIT is also influenced by numerous external and internal, host-related factors. External factors include the microbial load of the immediate environment, type of food eaten, and feeding habits, in addition to the composition of the maternal microbiota. Also, dietary and temperature-related stresses can influence the succession of microbes.8 Internal factors include, but are not limited to, intestinal pH; microbial interactions; environmental temperature; physiological factors, such as peristalsis; bile acids; host secretions and immune responses; drug therapy; and bacterial mucosal receptors.8
Given the abundance of factors that influence the composition of the intestinal microbiota, it is perhaps unexpected that the composition of the microbial community in the human gut is fairly stable at the phylum level.10 The Bacteroidetes and Firmicutes are conserved in virtually all individuals, although the relative proportions of these phyla may vary.5 However, when considered at the level of bacterial species, the variation in the composition of interindividual microbial communities is considerably greater than that observed at the phylum level.11 The potential explanation for this fact appears to be found within the deep functional redundancy inherent to the gut microbiota.5 The host generates a selective pressure to maintain certain functions within the GIT, and these functions may be attributed to a large number of bacterial species within the major phyla. Functional redundancy is the ability of one microbial group to carry out a functional process at the same rate as another under the same conditions, rather like a backup option, which allows for variations in the composition of the microbiota between individuals without compromising the maintenance of complete function within a particular individual.10
Bacterial cells are unevenly distributed along the length of the GIT. The numbers of bacteria present can vary, beginning at between 10 to 103 bacteria per gram of stomach and duodenal contents, increasing to between 104 and 107 bacteria per gram in the small intestine, and rising to between 1011 and 1012 bacteria per gram in the large intestine.10 Moreover, the composition of the microbial community varies among these sites, with different bacterial phyla enriched in the small intestine and colon. When biopsy samples from both regions in the gut of healthy individuals were examined, the small intestine was found to be enriched for certain members of the Firmicutes phyla and the colon for members of the phylum Bacteroidetes.12
Coupled with microbial heterogeneity along the length of the GIT, a large number of variations existed in the composition of the microbiota when intestines were studied in transverse section.13 Several microenvironments existed across the intestine, and the microbiota in the lumen of the intestine differed significantly in their composition from the microbiota in close proximity and attached to the epithelium. For example, the genera Bacteroides, Bifidobacterium, Streptococcus, Enterococcus, Clostridium, Lactobacillus, and Ruminococcus were all found in the feces, making the composition representative of the luminal community, whereas only Clostridium, Lactobacillus, and Enterococcus were detected in the mucus layer and epithelial crypts of the small intestine.13
Functions of the Gut Microbiota
Metabolism
As the gut microbiota encode a substantively larger number of genes than its human host, it follows that they are able to undertake a variety of metabolic functions that humans are unable to do or are only able to do in a limited capacity. The gut bacteria are able to produce a variety of vitamins, synthesize all essential and nonessential amino acids, and carry out biotransformation of bile.14 In addition, the microbiome provides the vital biochemical pathways for the metabolism of nondigestible carbohydrates, which include large polysaccharides, such as resistant starches, cellulose, hemicellulose, pectins, and gums; some oligosaccharides that escape digestion; unabsorbed sugars and alcohols from the diet15; and host-derived mucins.16 This functionality results in the recovery of energy and absorbable substrates for the host and a supply of energy and nutrients for bacterial growth and proliferation.17 Metabolism of carbohydrates is a major source of energy in the colon.
Host Protection and Immune-system Development
Many intestinal bacteria produce antimicrobial compounds and compete for nutrients and sites of attachment in the gut lining, thereby preventing colonization by pathogens. This action is known as the barrier or competitive-exclusion effect. Host cells in the gut wall have attachment sites that can be used by pathogenic bacteria to enter the epithelial cells. In laboratory studies, nonpathogenic bacteria can be seen to compete for these attachment sites in the border of intestinal epithelial cells, preventing the attachment and subsequent entry of pathogenic, enteroinvasive bacteria into the epithelial cells.17 Further, because bacteria compete for nutrients in their immediate surroundings and maintain their collective habitat by administering and consuming all resources, the enteric microbiota can outcompete pathogenic bacteria for resources, by sheer force of numbers.17 In addition, bacteria can inhibit the growth of their competitors by producing antimicrobial substances known as bacteriocins, and the ability to synthesize these bacteriocins is widely distributed among gastrointestinal bacteria.17
The intestinal epithelium is the main interface between the immune system and the external environment. The development of a host’s immune system is affected by continuous and dynamic interactions with the intestinal microbiota and its metabolites. Bacteria are integral to the early development of the gut-mucosal immune system, both in terms of its physical components and its function, and continue to play a role later in life in its operation.17 The cells of the intestinal epithelium avert threats from pathogens by signaling to the innate immune system through specific receptors14 that recognize and bind to specific molecules associated with bacteria, leading to the production of a host’s immune response and the release of protective peptides, cytokines, and white blood cells. The result can be a protective response to commensal bacteria, an inflammatory response to pathogenic organisms, or a trigger for a host’s cell death.
Exposure to intestinal bacteria is also implicated in the prevention of allergy (ie, a disproportionate reaction of the immune system to nonharmful antigens). Allergic infants and young children have been found to have a different composition of intestinal bacteria than those who do not develop allergies. It is hypothesized that the intestinal microbiota stimulates the immune system and trains it to respond proportionately to all antigens. An altered composition of intestinal microbiota in early life can lead to an inadequately trained immune system that can, and often does, overreact to antigens.18
The Gut–Brain Axis
The gut–brain axis is a communication system that integrates neural, hormonal, and immunological signaling between the gut and the brain, offering the intestinal microbiota and its metabolites a potential route through which to access the brain.19 This communication system is bidirectional, which enables the brain to command gastrointestinal functions, such as peristalsis and mucin production, and immune functions.20 Significant progress has been made over the past decade in recognizing the important ways in which gut microbiota relate to brain function.21 Foster and McVey Neufeld21 have reviewed key findings, showing that stress influences the composition of the gut microbiota and that bidirectional communication between the gut microbiota and the central nervous system influences a host’s stress reactivity. Stress has been shown to influence the integrity of the gut epithelium and to alter peristalsis, secretions, and mucin production, thereby altering the habitat of the intestinal microbiota and promoting changes in microbial composition and/or metabolism.19
Gut Microbiota in Disease
Associations have been established between human intestinal microbiota and a seemingly ever-increasing number of diseases, syndromes, and functional aberrations. The support for these associations varies from anecdotal reports from individuals to results from large cohort studies. The next section focuses on summarizing the associations that have garnered the greatest amount of attention: the possibility of a link between the intestinal microbiota and (1) chronic gastrointestinal diseases such as IBS and IBD, and (2) systemic metabolic diseases, such as type 2 diabetes and obesity.
Irritable Bowel Syndrome
IBS is defined as a group of functional bowel disorders in which abdominal discomfort or pain is associated with defecation or a change in bowel habits and with features of disordered defecation. Medical practitioners have agreed to further classification according to the Rome 3 criteria22 and have categorized the disease on the basis of a patient’s stool characteristics (Table 1).
Table 1
Etiological Classification of Symptoms of IBS
| IBS Subtype | Characteristics | |
| IBS with diarrhea | IBS-D |
|
| IBS with constipation | IBS-C |
|
| Mixed or cycling | IBS IBS-M |
|
| Unsubtyped IBS |
|
Abbreviation: IBS = irritable bowel syndrome.
IBS is thought to affect approximately 10% to 20% of adults and adolescents worldwide.22 The exact cause of IBS is unknown and is thought to be multifactorial. Genetic factors, motor dysfunction of the GIT, visceral hypersensitivity, infection, inflammation, and immunity as well as psychopathological factors are thought to play roles in its development.23 Together with these factors, variation in the gut microbiota is thought to be complicit in the low-grade intestinal inflammation associated with the syndrome.24 In the healthy gut, the intestinal microbiota either have direct bactericidal effects or can prevent the adherence of pathogenic bacteria to the wall of the GIT.25 In addition, dysbiosis (ie, microbial imbalance) in the gut may facilitate the adhesion of enteric pathogens that may be associated with IBS symptoms.26 Alteration in the composition of the normal microbiota and disturbed colonic fermentation in IBS patients may play an important role in development of IBS symptoms, with a significant, 2-fold increase in the ratio of Firmicutes to Bacteroidetes reported in IBS patients.27
Inflammatory Bowel Disease
IBD encompasses Crohn’s disease (CD) and ulcerative colitis (UC). CD is characterized by a cobblestone-like pattern of inflammation (ie, affected regions interrupted by healthy tissue), which can occur anywhere along the length of the GIT. It is also typified by ulcerations that may span the entirety of the intestinal wall, resulting in fissures that may perforate the intestinal wall and impact other organs such as the kidney or uterus.28 UC typically manifests as contiguous inflammation involving only the surface layers of the intestinal wall. It is primarily localized in the colon and most commonly originates at the rectum.29
Although individual microbial species may play significant roles in immunomodulation, aberration of the gut microbiome due to loss or overabundance plays a key role in the persistence of inflammatory responses in chronic disease. The role of the gut microbiota in IBD pathogenesis has been demonstrated by studies showing that antibiotic use can reduce or prevent inflammation, both in murine models of disease and in patients.30 Also, results from studies with UC patients inoculated with stool collected from healthy donors indicated disease remission within 1 week of receiving their fecal transfer, with complete recovery noted after 4 months.31
Similarly to IBS, IBD dysbiosis is concerned with large-scale alterations in the abundance and diversity of the Firmicute population, the relative abundance of which has been observed to be greatly reduced in IBD patients. The reduction in the numbers of Firmicutes is of particular interest because they are known producers of important short chain fatty acids (SCFAs), such as acetate and butyrate, that are known to have potent anti-inflammatory properties.32 Nagalingam and Lynch28 comprehensively reviewed the microbial alterations observed in IBD patients, detailing myriad microbial outcomes in different individuals and studies, with no apparent conclusions on relevant microbial biomarkers or the microbial cause or effect of IBD.
Systemic Metabolic Diseases
Systemic metabolic diseases include obesity and type 2 diabetes. Early indications that the gut microbiota are involved in obesity came when metabolically obese mice, with a mutation in the leptin gene, were shown to have a significantly different microbiota compared with mice without the mutation.9 Further investigation indicated that the ratio of Firmicutes to Bacteroidetes in the gut microbiota of obese mice was shifted in favor of Firmicutes, whereas lean mice were dominated by Bacteroidetes.33 In more recent human studies, the researchers found that the composition of the gut microbiota was altered in obese when compared with normal-weight individuals and that the composition changed in response to changes in a host’s body weight.34 Subsequent studies have failed, however, to demonstrate a consistent relationship between obesity and the ratio of Firmicutes to Bacteroidetes at both the phylum and the species levels. These studies have been comprehensively reviewed by Tagliabue and Elli.35
Type 2 diabetes is a complex disorder influenced by both genetic and environmental elements, which has become a major public health concern throughout the world.36 Research studies investigating the underlying genetic contributors to type 2 diabetes mainly involve the use of genome-wide association studies focusing on identifying genetic components in a patient’s genome.37 Recently, research has indicated that the risks related to the development of type 2 diabetes may also involve the composition of the intestinal microbiota. The gut microbiota of participants with type 2 diabetes displayed only a limited deviation from the control group’s, although a decline in butyrate-producing bacteria that may be metabolically beneficial was observed.38 This observation suggests that a state of functional dysbiosis, rather than any specific microbial species, could have a direct association with the pathophysiology of type 2 diabetes. Increases in the presence of several categories of opportunistically pathogenic bacteria were also detected, although the abundance of these categories of opportunistic pathogens seemed to be quite variable.38
The gut microbiota is implicated in nutrient acquisition and energy harvest and produces exometabolites, such as SCFAs, that may regulate a host’s metabolic processes.39,40 SCFAs have been implicated in metabolic diseases, including obesity39 and type 2 diabetes.41 Higher levels of fecal SCFAs, mainly butyrate and propionate, have been reported in obese adults42 and children,43 when compared with lean individuals. Changes in the concentration and proportion of individual SCFAs may be in line with changes in the bacterial phyla present.42,43
A wealth of evidence now exists that indicates close ties between metabolic and immune systems, and the gut microbiota is being increasingly recognized as an important factor connecting genes, environment, and immune system. Among the many reasons to maintain a healthy weight is the emerging paradigm that metabolic imbalance leads to immune imbalance, with starvation and immunosuppression on one end of the spectrum and obesity and inflammatory diseases on the other end.36 It is possible that any dysbiosis that results in a disordered, rather than directional, alteration in the composition and functionality of gut microbials may itself have a role in increasing the susceptibility to a diseased state.38
Atopic Eczema and Other Allergic Disease
Allergic diseases, specifically those driven by type 1 hypersensitization—atopic eczema, atopic asthma, rhinitis—and type 1 food allergies have risen globally in incidence over the past 50 years, with the developed world now showing an incidence at 20% of the population, providing a considerable proportion of overall disease burden.44 Atopic sensitization occurs primarily in the first 2 years of life and can persist through a lifetime, with the expression of allergic disease typically beginning with eczema (0–2 y), asthma (>5 y), and rhinitis (>8 y) in what is referred to as the atopic march.45 Atopic eczema, an inflammatory skin condition, was found to affect up to 20% of children younger than 12 months of age in England and Wales during 200646 and cost the UK government nearly £500 million per annum in 1996.
The causes of atopic eczema are potentially numerous and are not well understood, although the method of birth (ie, vaginal vs cesarean) and a mutation in a particular human gene involved in skin-barrier function are known to be implicated.47 Characterization of the gut microbiota of sufferers of atopic eczema showed that infants at 1 month of age with the disease had a significantly lower bacterial diversity, particularly with regard to the Bacteroidetes phylum, compared with infants without atopic eczema.48 The study also highlighted decreased diversity of Bacteroidetes at 12 months of age in the atopic-eczema group, suggesting that sufferers may maintain a lower level of bacterial diversity when compared with healthy controls. In addition, a lower number of Proteobacteria, the cell walls of which contain lipopolysaccharide molecules, was observed in infants presenting with atopic eczema. Lipopolysaccharides have the ability to elicit a host’s immune response, and low exposure to lipopolysaccharides in infancy is linked with a higher risk of atopic eczema.49
As an explanation for the marked increase in allergic disease, the concept of reduced quantitative and qualitative exposure to the microbial world during the neonatal period has been termed the hygiene hypothesis and is based on the observation of increased atopy in smaller, and particularly urbanized, families50 from reduced exposure to microbial challenge. This underexposure to microbial antigens results in the aberrant outcome to allergen processing of immunological response rather than immunological tolerance.45
Conclusions and Perspective
The gut microbiota in humans evolve throughout life and appear to play a pivotal role in both health and disease. In a healthy state, the gut microbiota have myriad positive functions, including energy recovery from metabolism of nondigestible components of foods, protection of a host from pathogenic invasion, and modulation of the immune system. A dysbiotic state of the gut microbiota is becoming recognized as an environmental factor that interacts with a host’s metabolism and has a role in pathological conditions, both systemic—obesity, diabetes, and atopy—and gut-related IBS and IBD, although the specific contribution of the gut microbiota to these diseases is unclear. The heterogeneous etiology of metabolic and gastrointestinal diseases has been associated with different microbes, although little information exists about the causal direction of the association.
In the second part of this review, the authors will investigate interventions that have been shown to modulate and stabilize the gut microbiota and also to restore it to its healthy composition from the dysbiotic states seen in IBS, IBD, obesity, type 2 diabetes, and atopy.
References
- Harris MA, Reddy CA, Carter GR. Anaerobic bacteria from the large intestine of mice. Appl Environ Microbiol. 1976;31(6):907–912.
- Schloss PD, Handelsman J. Status of the microbial census. Microbiol Mol Biol Rev. 2004;68(4):686–691
- Claesson MJ, O’Sullivan O, Wang Q, et al. Comparative analysis of pyrosequencing and a phylogenetic microarray for exploring microbial community structures in the human distal intestine. PLoS One. 2009;4(8):e6669.
- Xu J, Gordon JI. Honor thy symbionts. Proc Natl Acad Sci U S A. 2003;100(18):10452–10459
- Lozupone CA, Stombaugh JI, Gordon JI, Jansson JK, Knight R. Diversity, stability and resilience of the human gut microbiota. Nature. 2012;489(7415):220–230. [PMC free article] [PubMed] [Google Scholar]
- Jiménez E, Marín ML, Martín R, et al. Is meconium from healthy newborns actually sterile? Res Microbiol. 2008;159(3):187–193. [PubMed] [Google Scholar]
- Huurre A, Kalliomäki M, Rautava S, Rinne M, Salminen S, Isolauri E. Mode of delivery—effects on gut microbiota and humoral immunity. Neonatology. 2008;93(4):236–240. [PubMed] [Google Scholar]
- Mackie RI, Sghir A, Gaskins HR. Developmental microbial ecology of the neonatal gastrointestinal tract. Am J Clin Nutr. 1999;69(5):1035S–1045S. [PubMed] [Google Scholar]
- Ley RE, Bäckhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102(31):11070–11075. [PMC free article] [PubMed] [Google Scholar]
- Sekirov I, Russell SL, Antunes LC, Finlay BB. Gut microbiota in health and disease. Physiol Rev. 2010;90(3):859–904. [PubMed] [Google Scholar]
- Eckburg PB, Bik EM, Bernstein CN, et al. Diversity of the human intestinal microbial flora. Science. 2005;308(5728):1635–1638. [PMC free article] [PubMed] [Google Scholar]
- Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780–13785. [PMC free article] [PubMed] [Google Scholar]
- Swidsinski A, Loening-Baucke V, Lochs H, Hale LP. Spatial organization of bacterial flora in normal and inflamed intestine: a fluorescence in situ hybridization study in mice. World J Gastroenterol. 2005;11(8):1131–1140. [PMC free article] [PubMed] [Google Scholar]
- Vyas U, Ranganathan N. Probiotics, prebiotics, and synbiotics: gut and beyond. Gastroenterol Res Pract. 2012;2012:872716. [PMC free article] [PubMed] [Google Scholar]
- Cummings JH, Pomare EW, Branch WJ, Naylor CP, Macfarlane GT. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut. 1987;28(10):1221–1227. [PMC free article] [PubMed] [Google Scholar]
- Koropatkin NM, Cameron EA, Martens EC. How glycan metabolism shapes the human gut microbiota. Nat Rev Microbiol. 2012;10(5):323–335. [PMC free article] [PubMed] [Google Scholar]
- Guarner F, Malagelada JR. Gut flora in health and disease. Lancet. 2003;361(9356):512–519. [PubMed] [Google Scholar]
- Björkstén B, Sepp E, Julge K, Voor T, Mikelsaar M. Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol. 2001;108(4):516–520. [PubMed] [Google Scholar]
- Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012;10(11):735–742. [PubMed] [Google Scholar]
- Mayer EA. Gut feelings: the emerging biology of gut-brain communication. Nat Rev Neurosci. 2011;12(8):453–466. [PMC free article] [PubMed] [Google Scholar]
- Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305–312. [PubMed] [Google Scholar]
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–1491. [PubMed] [Google Scholar]
- Ghoshal UC, Shukla R, Ghoshal U, Gwee KA, Ng SC, Quigley FM. The gut microbiota and irritable bowel syndrome: friend or foe? Int J Inflam. 2012;2012:151085. [PMC free article] [PubMed] [Google Scholar]
- Guinane CM, Cotter PD. Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therap Adv Gastroenterol. 2013;6(4):295–308. [PMC free article] [PubMed] [Google Scholar]
- Kellow JE, Azpiroz F, Delvaux M, et al. Applied principles of neurogastroenterology: physiology/motility sensation. Gastroenterology. 2006;130(5):1412–1420. [PubMed] [Google Scholar]
- Rinttilä T, Lyra A, Krogius-Kurikka L, Palva A. Real-time PCR analysis of enteric pathogens from fecal samples of irritable bowel syndrome subjects. Gut Pathog. 2011;3(1):6. [PMC free article] [PubMed] [Google Scholar]
- Ponnusamy K, Choi JN, Kim J, Lee SY, Lee CH. Microbial community and metabolomic comparison of irritable bowel syndrome faeces. J Med Microbiol. 2011;60(pt 6):817–827. [PMC free article] [PubMed] [Google Scholar]
- Nagalingam NA, Lynch SV. Role of the microbiota in inflammatory bowel diseases. Inflamm Bowel Dis. 2012;18(5):968–984. [PubMed] [Google Scholar]
- Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369(9573):1641–1657. [PubMed] [Google Scholar]
- Swidsinski A, Weber J, Loening-Baucke V, Hale LP, Lochs H. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J Clin Microbiol. 2005;43(7):3380–3389. [PMC free article] [PubMed] [Google Scholar]
- Borody TJ, Warren EF, Leis SM, Surace R, Ashman O, Siarakas S. Bacteriotherapy using fecal flora: toying with human motions. J Clin Gastroenterol. 2004;38(6):475–483. [PubMed] [Google Scholar]
- Barcenilla A, Pryde SE, Martin JC, et al. Phylogenetic relationships of butyrate-producing bacteria from the human gut. Appl Environ Microbiol. 2000;66(4):1654–1661. [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–1131. [PubMed] [Google Scholar]
- Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489(7415):242–249. [PubMed] [Google Scholar]
- Tagliabue A, Elli M. The role of gut microbiota in human obesity: recent findings and future perspectives. Nutr Metab Cardiovasc Dis. 2013;23(3):160–168. [PubMed] [Google Scholar]
- Wellen KE, Hotamisligil GS. Inflammation, stress, and diabetes. J Clin Invest. 2005;115(5):1111–1119. [PMC free article] [PubMed] [Google Scholar]
- Scott LJ, Mohlke KL, Bonnycastle LL, et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science. 2007;316(5829):1341–1345. [PMC free article] [PubMed] [Google Scholar]
- Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55–60. [PubMed] [Google Scholar]
- Nicholson JK, Holmes E, Kinross J, et al. Host-gut microbiota metabolic interactions. Science. 2012;336(6086):1262–1267. [PubMed] [Google Scholar]
- Fernandes J, Su W, Rahat-Rozenbloom S, Wolever TM, Comelli EM. Adiposity, gut microbiota and faecal short chain fatty acids are linked in adult humans. Nutr Diabetes. 2014 Jun;4:e121. [PMC free article] [PubMed] [Google Scholar]
- Kaczmarczyk MM, Miller MJ, Freund GG. The health benefits of dietary fiber: beyond the usual suspects of type 2 diabetes mellitus, cardiovascular disease and colon cancer. Metabolism. 2012;61(8):1058–1066. [PMC free article] [PubMed] [Google Scholar]
- Schwiertz A, Taras D, Schäfer K, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring) 2010;18(1):190–195. [PubMed] [Google Scholar]
- Payne AN, Chassard C, Zimmermann M, Müller P, Stinca S, Lacroix C. The metabolic activity of gut microbiota in obese children is increased compared with normal-weight children and exhibits more exhaustive substrate utilization. Nutr Diabetes. 2011 Jul;1:e12. [PMC free article] [PubMed] [Google Scholar]
- Okada H, Kuhn C, Feillet H, Bach JF. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160(1):1–9. [PMC free article] [PubMed] [Google Scholar]
- Shen CY, Lin MC, Lin HK, Lin CH, Fu LS, Fu YC. The natural course of eczema from birth to age 7 years and the association with asthma and allergic rhinitis: a population-based birth cohort study. Allergy Asthma Proc. 2013;34(1):78–83. [PubMed] [Google Scholar]
- Schofield JK, Fleming D, Grindlay D, Williams H. Skin conditions are the commonest new reason people present to general practitioners in England and Wales. Br J Dermatol. 2011;165(5):1044–1050. [PubMed] [Google Scholar]
- Williams HC, Grindlay DJ. What’s new in atopic eczema? An analysis of systematic reviews published in 2007 and 2008, I: definitions, causes and consequences of eczema. Clin Exp Dermatol. 2010;35(1):12–15. [PubMed] [Google Scholar]
- Abrahamsson TR, Jakobsson HE, Andersson AF, Björkstén B, Engstrand L, Jenmalm MC. Low diversity of the gut microbiota in infants with atopic eczema. J Allergy Clin Immunol. 2012;129(2):434–440. [PubMed] [Google Scholar]
- Gehring U, Bolte G, Borte M, et al. LISA study group. Lifestyle-Related Factors on the Immune System and the Development of Allergies in Childhood. Exposure to endotoxin decreases the risk of atopic eczema in infancy: a cohort study. J Allergy Clin Immunol. 2001;108(5):847–854. [PubMed] [Google Scholar]
- Strachan DP. Hayfever, hygiene, and household size. BMJ. 1989;299(6710):1259–1260. [PMC free article] [PubMed] [Google Scholar]

