ACTIVATE YOUR VAGUS NERVE – UNLEASH YOUR BODY’S NATURAL ABILITY TO HEAL
Gut Sensitivities, Inflammation, Brain Fog, Autoimmunity, Anxiety, Depression, Dr. Navaz Habib, Ulyssess Press, Berkely California, 2019
Summary written by Ronald Peters MD, MPH, MindBody Medicine Center
PART 1: WHAT IS THE VAGUS NERVE?
PART 2: WHAT IS THE PATH AND FUNCTION OF THE VAGUS?
PART 3: WHAT COULD GO WRONG WITH THE VAGUS?
PART 4: HOW DO YOU MEASURE AND ACTIVATE THE VAGUS?
PART 1: WHAT IS THE VAGUS NERVE?
 The vagus nerve is the conductor of the human body symphony orchestra.
The vagus nerve is the conductor of the human body symphony orchestra.
Your heart will beat 100,000 times today and you will take 23,000 breaths. Your blood will circulate through your body three times per minute, and your liver will continuously cleanse and detoxify that blood. The ever-changing population of bacteria in your gut will work symbiotically with your digestive tract to break down your food and absorb the nutrients required for each of your cells to function.
And this natural body wisdom occurs automatically, and you do not have to think about it. The autonomic nervous system is an evolutionary marvel and is responsible for the control of bodily functions so you can about your day.
The vagus nerve originates in the brain and regulates the vast majority of the automatic functions of the body. These functions are called autonomic and are regulated by your autonomic nervous system.
THE AUTONOMIC NERVOUS SYSTEM CONTROLS THE FOLLOWING:
- Beating of the heart
- Blinking of eyelids
- Breath rate and depth
- Constriction and dilation of blood vessels
- Detoxification in the liver and kidneys
- Digestion in the digestive tract
- Opening and closing sweat glands
- Producing saliva and tears
- Pupil dilation and constriction in eyes
- Sexual arousal
- Urination
 The vagus nerve is the neurological highway that connects the organs of the body with the brain. Eighty percent of the information transmitted by the vagus nerve is “afferent”, or, incoming from the heart, lungs, and digestive tract for the brain. The remaining 20 percent of the neurons in the vagus highway have an “efferent signal”, from the brain to the body in order to optimize the function of the organs in the body.
The vagus nerve is the neurological highway that connects the organs of the body with the brain. Eighty percent of the information transmitted by the vagus nerve is “afferent”, or, incoming from the heart, lungs, and digestive tract for the brain. The remaining 20 percent of the neurons in the vagus highway have an “efferent signal”, from the brain to the body in order to optimize the function of the organs in the body.
Managing the inflammatory system is one of the most important functions of the vagus nerve. The vagus is the major inflammatory control system in the body and has far-reaching effects on your personal state of health and disease. Many of the health conditions that my patients suffer from are due to high levels of inflammation in certain organs and systems, from the digestive tract to the liver and even the brain. Inflammation is a protective and healthy response within the body to keep us safe from bacterial and viral invaders, physical trauma, and other things that should optimally not enter the body. When inflammation becomes chronic, the effects can be wide-ranging and lead to many different health conditions.
SOME COMMON CONDITIONS CORRELATED TO HIGH INFLAMMATION LEVELS INCLUDE:
- Alzheimer’s disease
- Arthritis
- Asthma
- Cancer
- Crohn’s disease
- Diabetes
- Heart and cardiovascular disease
- High blood pressure
- High cholesterol
- Postural orthostatic tachycardia syndrome (POTS)
- Ulcerative colitis
- As well as any condition that ends in the suffix –it is
PART 2: WHAT IS THE PATH AND FUNCTION OF THE VAGUS?
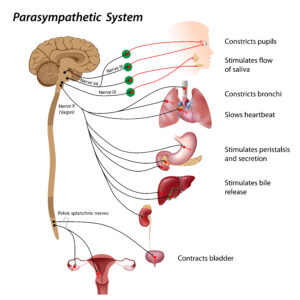
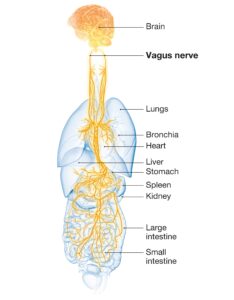
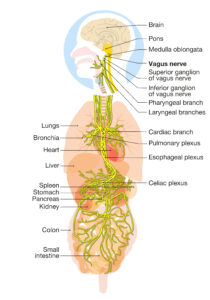 The vagus nerve is the longest nerve in the body. it originates deeply within the brain and sends signals to the body through other branches of the parasympathetic fibers of the vagus, which serve to calm and regulate the function of the heart and lungs and increase the action of the gut and intestinal tract, liver, pancreas, gallbladder, and spleen.
The vagus nerve is the longest nerve in the body. it originates deeply within the brain and sends signals to the body through other branches of the parasympathetic fibers of the vagus, which serve to calm and regulate the function of the heart and lungs and increase the action of the gut and intestinal tract, liver, pancreas, gallbladder, and spleen.
As the nerve leaves the brain in enters the carotid sheath in the neck near internal carotid artery and internal jugular vein, the vagus nerve is given extra soft tissue protection as it passes down through the neck.
Within the carotid sheath, the vagus nerve gives off its next branch: the pharyngeal branch. The pharyngeal branch has neurons from the vagus nerve but also carries some contributing neurons from the ninth and eleventh cranial nerves (glossopharyngeal and accessory nerves). Once these neurons converge, they will pass toward the midline of the body until they reach the upper part of the throat, called the pharynx. In the pharynx, the vagus nerve relays motor signals to multiple muscles that are involved in the swallowing reflex, managing the opening and closing of the upper airway, and maintaining the gag reflex.
Now, let’s follow the path of the nerves from the brainstem downward into the neck, thorax (chest area), and abdomen (belly area).
The first branch of the vagus is called the auricular branch. extends toward the skin of each ear. This branch senses touch, temperature, and wetness on the skin of the ear; specifically, the external canal, tragus, and auricle. It is the main target for vagal nerve activation treatment using auricular acupuncture (acupuncture points in the ear).
As the nerve continues its journey into the body it thickens to form the inferior ganglion, also known as the nodose ganglion. The cell bodies at this location are involved in bringing information from the internal organs. The nerve then thins out again and immediately enters a passageway created by a thickening of connective tissue called the carotid sheath.
Within the carotid sheath, the vagus nerve gives off its next branch: the pharyngeal branch, which reaches the upper part of the throat, called the pharynx. At this location , the vagus nerve relays motor signals to multiple muscles that are involved in the swallowing reflex, managing the opening and closing of the upper airway, and maintaining the gag reflex.
As the vagus nerve descends the sides of the neck within the carotid sheath, it gives rise to the third branch, known as the superior laryngeal nerve. This nerve supplies motor control to the muscles of the larynx above the vocal cords, specifically the muscles that control the pitch of your voice.
As the vagus courses down through the carotid sheath, it gives rise to the cervical cardiac branches, which are two of the three branches that innervate the heart. The third branch, the thoracic cardiac branch, arises soon after leaving the carotid sheath in the chest (thorax) area. These branches intermingle with nerves of the sympathetic nervous system and form the cardiac plexus (a plexus, pluralized as plexi, is a collection of
intermingling nerve fibers of different branches and different origin nerves that courses toward a specific location). We have two cardiac plexi: one in front of the aorta called the superficial cardiac plexus, and one behind the arch of the aorta called the deep cardiac plexus. (The aorta is the primary blood vessel, which carries blood from the heart to the rest of the body.)
Some fibers of the cardiac plexi extend toward the sinoatrial node of the heart, while others will extend toward the atrioventricular (AV) node. We will discuss the function of these nerves on the heart in the next chapter. For now, the most important thing to remember is that these fibers control the rate of electrical activity that pumps your heart.
INTO THE CHEST
After the nerve exits the bottom of the carotid sheath, it courses downward into the thorax, behind the first and second ribs, and in front of the larger blood vessels that extend from the heart.
The left vagus nerve passes in front of (anterior to) the arch of the aorta and then sends off its fourth branch—the recurrent laryngeal nerve. On the opposite side of the body, the right vagus nerve follows a similar path; however, it passes in front of the right subclavian artery and then sends off its fourth branch, the right side recurrent laryngeal nerve.
 Both recurrent laryngeal nerves follow a similar path, but on opposite sides of the body. These are the only branches of the nerve that turn and course upward toward the neck again. They carry motor signals from the brainstem to each of the larynx muscles below the vocal cords, which are important for the production of vocal sounds, based on tensioning and loosening of the vocal cords.
Both recurrent laryngeal nerves follow a similar path, but on opposite sides of the body. These are the only branches of the nerve that turn and course upward toward the neck again. They carry motor signals from the brainstem to each of the larynx muscles below the vocal cords, which are important for the production of vocal sounds, based on tensioning and loosening of the vocal cords.
Once the nerves reach the level of the aorta, each one of the vagus nerves sends off branches to the next pair of organs, the lungs. The left vagus nerve sends a pulmonary branch to the anterior pulmonary plexus and the right vagus nerve sends a pulmonary branch to the posterior pulmonary plexus. These nerve branches mix with sympathetic neurons, reorganize, then travel to each side to innervate the lungs. These branches go to the bronchi and larger branches of the lungs to open and close them according to the need of the body based on each situation.
One organ in the thorax that the vagus nerve innervates is often highly overlooked or forgotten about: the thymus. The thymus is an extremely important organ of the immune system. It is located in the mediastinum of the chest, in front of the heart but behind the sternum. A branch of the vagus makes its way to this nerve to send signals to and from the thymus. The thymus forms early in our development and is the major source of training for and growth of our white blood cells. The reason this organ is so easily forgotten is that over time, it shrinks and is replaced by fat tissue. This process begins during puberty and can continue for many years into early adulthood. I like to think of the thymus as a school for new immune cells, and as the school gets old and deteriorates, the training that the white blood cells go through decreases in quality. We will discuss the role of the thymus in much greater detail in later chapters.
INTO THE ABDOMEN
The final section that the vagus nerve innervates is the organs of the abdomen. These organs are important for digestion, controlling the immune system, and ensuring that the blood reaching the rest of our cells does not contain toxins that can negatively affect cell health.
The first abdominal branch of the vagus nerve goes to the stomach. When our body is in the rest-and-digest state, the fibers of the vagus nerve stimulate stomach muscles to function. They send signals to the parietal cells to produce and secrete hydrochloric acid (HCI), the chief cells to produce and secrete the digestive enzymes pepsin and gastrin, and the smooth muscle cells of the stomach to physically churn and push the food in our stomach into the next section of the digestive tract, the small intestine.
If the vagus nerve is damaged and does not send these important signals to the cells of the stomach, it will lead to issues such as hypochlorhydria, or low stomach acid, which is a major root cause of many health conditions. Sufficiently low pH (high acid) is needed for activating digestive enzymes and breaking down food. The optimal range of stomach pH should be around 3.0 in the stomach, while nothing above 5.0 will be strong enough to
activate pepsin and gastrin. Low stomach acid makes food breakdown less optimal. Higher pH in the stomach can also allow unwanted bacteria, viruses, and parasites to make their way into the intestines and wreak havoc on your digestive tract.
The second abdominal branch of the vagus goes to the liver. Interestingly, these branches are strongly linked to the sensation of hunger and desire for certain types of nutrients. The food that we eat initially enters the stomach to be broken down. It then enters the small intestine, where most of our macronutrients (fats, carbohydrates, and amino acids from protein) are absorbed into the bloodstream. These nutrients then flow into the liver via the portal vein for filtration, processing, and sending signals back up to the brain.
From the liver, the vagus relays information to the brain regarding blood sugar balance, intake of fats, and overall liver function. The vagus nerve can also relay information regarding the amount of bile necessary to help in the digestion of fats. The liver has many functions that require vagus input, including:
- production of bile and bile salts (the active component of bile),
- balancing the blood sugar through production of glucose;
- managing hunger and satiety through the measurement of fat intake;
- filtration of blood in the portal vein, which brings all nutrients and toxins from the gut; and
- phase 1 and phase 2 of detoxification processes for fat-soluble hormones, neurotransmitters, and toxins from the body.
The liver is very important to our overall well-being and vagus innervation is strongly associated with maintaining this balance.
The vagal nerve is Intimately connected to the liver is the gallbladder which is important for optimal function of our bodies. When the liver creates bile and bile salts, they are sent to the gallbladder for storage in preparation for the next meal. When the next meal occurs, the gallbladder pumps bile into the duodenum (the first part of the small intestine) to help bring fats into the bloodstream. The pump of the gallbladder is mediated by the vagus nerve. From the liver, the vagus branches off to send signals to the gallbladder, activating the smooth muscle cells in its walls to pump bile into the digestive tract. This happens in response to a meal that the taste buds (sensory receptors on the tongue) determined contained fat, which should be digested once it reaches the small intestine.
The next branch of the vagus is directed toward the pancreas. Your pancreas is one of the most important glands in your body, with both an exocrine and endocrine component. The endocrine pancreas produces and secretes insulin and glucagon directly into the bloodstream to balance glucose levels in the blood (blood sugar). The exocrine pancreas produces and secretes digestive enzymes through a duct directly into the small intestine. The three most notable digestive enzymes produced by the pancreas are protease, which breaks down proteins into their component amino acids; lipase, which breaks down fats from their component triglycerides into free fatty acids and cholesterol; and amylase, which breaks down carbohydrates into simpler sugars.
Vagus innervation sends signals from the pancreas back to the brainstem, relaying information regarding exocrine and endocrine cell status. It also relays information from the brainstem back to the organ regarding food intake and which enzymes are required for production and release into the bloodstream and digestive tract. Vagus innervation is essential for relaying this information because a lack of signaling will alter the release of digestive enzymes, reducing the effectiveness of the digestive process. Once the vagus nerve courses past the stomach, it forms the celiac plexus, which is a network formed between lumbar sympathetic nerves and the parasympathetic fibers of the vagus. This network sends branches to the remaining organs in the abdomen.
The first organ innervated after the celiac plexus is the spleen. The spleen is located on the left side of your body, below the left lung, opposite the liver. Its function is to monitor the bloodstream and activate or deactivate cells of the immune system based on what it senses. Early in our lives, both the spleen and the thymus manage immune cell function, but later in life once the thymus has disappeared, this system is managed by just the spleen.
The spleen receives messages from the sympathetic branches to activate the inflammatory pathways, which turn on in response to physical and biochemical trauma or damage. The parasympathetic branches send signals to halt the inflammation processes. The vagus nerve modulates a system called the cholinergic anti-inflammatory pathway, which has major effects in the spleen. We will discuss these specific effects in later sections related to inflammation.
The next branch of the vagus after the celiac plexus travels to the small intestine. Once food has been broken down by the chemical and physical churning in the stomach, it enters the small intestine. Here it undergoes further digestive processing by pancreatic digestive enzymes and bile. The function of the small intestine is to break down and absorb most of our macronutrients. These include fats, carbohydrates, and proteins (which are ideally broken down into their component amino acids). The bloodstream receives the macronutrients that have been accepted by the lining cells of the small intestine.
The bite of food that we take (which is called chyme at this point in the digestive process) must be pushed along the winding and coursing length of the small intestine. For this to happen, the vagus nerve activates the smooth muscle cells of the digestive tract by signaling the extensive network of nerves that line the gut, called the enteric nervous system.
Contrary to its name, the small intestine is actually very long, approximately 22 feet long, and significantly longer than the next portion of the digestive tract, the large intestine.
We have an immensely important relationship with the other cells that are living within our digestive tracts. I am speaking of the symbiotic relationship between our human cells and the bacteria that are living in our gut: our microbiome. Most of our bacterial allies live in our large intestine—the thicker, shorter area of the digestive tract. Although these bacteria produce many important vitamins, minerals, and biochemical precursors for us, they can also produce many toxins and gas. We require a system that can keep these bacteria in check and relay signals to our brain regarding the status of digestive tract and microbiome function. So, while the vagus nerve activates smooth muscle cells to push food along the remainder of the digestive tract, it is also the major relay path for the microbiome to speak with the brain. The vagus nerve innervates approximately the first half of the large intestine—the ascending and transverse portions.
The final organ innervated by the vagus nerve is actually two organs, with one located on each side of the body—the kidneys. These organs have a few different functions that are crucial to our health. The kidneys filter fluid out of the body in the form of urine, a combination of uric acid and water, which is then sent down to the bladder. One of the major determinants of this control is blood pressure, which will be discussed further in the next chapter. The vagus nerve is a major controller of the function of the kidneys and thus has a major role in the management of blood pressure.
At the end of its course, the vagus nerve does not simply end. Rather, it forms a final plexus with the parasympathetic nerves that course from the lower end of the spinal cord. These parasympathetic fibers innervate the second half of the large intestine, called the descending and sigmoid colon, as well as the bladder and sex organs.
THE FUNCTIONS OF THE VAGUS NERVE
An optimally functioning VN is essential for optimizing health and halting the progression of disease.
The vagus nerve is the conductor of the incredibly complex biological symphony that is your body. It operates every second of your life so you can live as you choose. It regulates the function of your lungs, heart and digestive system based on complex data analysis and feedback. When it is functioning optimally it can sense activity and send control commands to the many organs and cells of the body. Dysfunctional signaling will lead to dysharmony and eventually to chronic disease, which is epidemic, afflicting 60% of Americans.
Sensing Skin of the Ear
The first branch of the vagus nerve is the auricular branch, which is specifically involved in sensing the skin of the auricle, tragus, and external auditory canal of the ear.
Our ears are sensitive to the environment to stay alert and survive. The function of this branch is sensation, allowing us to feel pressure, touch, temperature, and moisture on the central section of each ear. The vagus nerve can be stimulated using techniques such as acupuncture.
Allowing Food to Be Swallowed
The process of swallowing without choking is managed by the vagus nerve.
The second branch of the vagus activates the five muscles of the pharynx. These muscles push chewed food toward the larynx and the esophagus while keeping it out of the trachea, thus keeping the airway clear of food. This branch of the vagus also manages the gag reflex.
Poor vagus nerve function will lead to coughing and a change in the function of the gag reflex.
Managing Your Airway and Vocal Cords
The vagus keeps your upper airway open and are also involved in the production of voice – they ensure the powerful experience of verbal communication.
Vagal nerve dysfunction results in a change in pitch and can become a chronically hoarse voice or an easily fatigued, monotonous voice. This is another sign of poor vagal tone. Irritation or malfunction of this branch of the vagus can also result in cough and risk of aspiration (i.e., food or drink entering the trachea through the impaired function of the vocal cords).
In addition to hoarseness, dysfunction of these nerves can leads to loss of voice, and trouble breathing during physical activity. Any difficulty with breathing or speaking may be the due to decreased vagus nerve function and tone.
Controlling Breathing
The pulmonary branch of the vagus runs to the pulmonary plexus and connects with the sympathetic nervous system and innervates the trachea and the bronchi of both lungs. The vagus component is a sensory nerve that relays information to the brain regarding lung expansion levels, as well as oxygen and carbon dioxide levels.
Vagus nerve activation slows the breathing rate and deepens the breath. During the parasympathetic, rest-and-digest phase, breathing tends to be deeper and the rate of the breath tends to be lower. When a person is transitioning from a fight-or-flight state into a rest-and-digest phase, a slow, deep breath rate will activate the vagus nerve and stimulate the relaxation reflex.
Vagus tone is necessary for opening the airway in the pharynx, larynx, and trachea. Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea are both signs of low vagal tone and a need for vagus nerve activation.
Controlling Heart Rate
The vagus nerve has a major role in ensuring that the heart rate stays at an optimal rate for the various conditions we encounter.
The vagus nerve is directly connected to the sinoatrial node, which sends electrical signals to the two atria (the thinner chambers at the top of the heart). It is also directly connected to the atrioventricular node, which manages the pumping rate and contraction pressure of the ventricles (the two thicker, lower chambers of the heart).
During times of fight-or-flight, the sympathetic nervous system the vagus activates the heart to increase pumping rate and the pressure of the contractions in the two ventricles. When the stressor has passed, the parasympathetic fibers of the vagus slow the heart rate and actively decrease the pressure of pumping contractions. This cardiac control allows the heart to rest and recover from times of stress and severe activation.
Maintaining Optimal Blood Pressure
The kidneys function to filter fluid and toxins out of the body and are thus the body’s major blood pressure manager. The vagus nerve relays information to and from the kidneys to help it manage the flow of water and fluid from within the kidney glomeruli, the basic filtration unit of the kidney, thus managing the overall blood pressure of the body. When the body is under stress, signals from the blood vessels are relayed up the brainstem and back down to the kidneys via the vagus and sympathetic nerves. The kidneys then constrict their blood vessels and increase blood pressure by reducing the amount of water being filtered out of the bloodstream. When the body is relaxed, signals from the carotid body tell the kidneys to filter out more water and to dilate the blood vessels to decrease blood pressure.
Hormones are also intimately connected to this process, working with the vagus and sympathetic nerves. However, the immediate control comes from the nerves and the slow, gradual management is determined by the hormones.
High blood pressure is a very common diagnosis and medications are often prescribed to control these levels. High blood pressure can be a sign of overactivation of stress hormones of the adrenal glands, and the stress response, which is mediated through sympathetic nerves. It is also a very common sign of vagus nerve dysfunction and poor vagal tone.
Controlling the Many Functions of the Liver
The vagus nerve relays much important information to and from the liver, managing its 500 tasks to help us manage nutrients and detoxify the body.
During times of stress, when the body shifts into fight-or-flight mode, blood flow is pushed toward the arms and legs to increase muscle activation and allow us to fight off an attack, or to run away from it. Blood flow in the liver will decrease, as digestion and blood filtration during this stressful event are not a priority for survival. When the body is relaxed in the rest and-digest phase, vagus nerve activation increases and blood flow to the liver will increase. During these times, digestion, filtration of blood, and other functions for cellular thriving are prioritized.
The vagus nerve also controls the cells in the liver that are responsible for producing bile, as well as transporting bile into the gallbladder and small intestine. It has been shown that when the vagus nerve is active, these cells, called cholangiocytes, are active and increase the flow of bile into the gallbladder for storage.
Bile performs multiple functions for the liver and the body. Bile holds toxins that have been rendered harmless and are ready to be released from the body through the digestive tract via our stool. Stool is only one of three routes by which the waste products are released. The other methods of waste elimination are urine via the kidneys or as sweat via the skin.
Bile salts, the effective component of bile, have another role. When bile is released into the small intestine, it releases waste products and bile salts. The bile salts are required to escort triglycerides (molecules of fat) from the digestive tract and into the bloodstream. Without being escorted by bile salts, fats are not able to be absorbed, which is a bad thing, because fats and cholesterol have numerous vital functions in the body. This results in fatty stools, as well. The vagus nerve activates cholangiocytes and opens the flow of bile from the liver into the gallbladder, as well as from the gallbladder into the small intestine, ensuring that the essential nutrient fat can be absorbed.
WARNING ABOUT FAT: According to paleoanthropologists, our ancestors ate fat three times a week and we modern humans eat fat two or three times a day. Consequently, we develop insulin resistance and gain weight. As of 2019 41.0% of Americans were obese and another 31% were overweight. Obesity is not a fashion statement; it is a disease. Please refer to this link for more information.
. https://healmindbody.com/obesity-is-a-chronic-disease-according-to-the-american-medical-association/
Activating Gall Bladder Emptying
Once the liver has produced bile it is stored in the gall bladder where it matures, like a fine wine, until it is needed. Upon eating a meal, the taste buds in the tongue and rest of the mouth send signals to the brain, letting our body know about the macronutrients that it senses as part of each bite and the entirety of the snack or meal. If fats are being consumed, then the vagus nerve signals the liver and gallbladder that bile will be needed soon.
Upon receiving this signal, the gallbladder will activate the smooth muscle cells in its lining and pump the bile out through the bile duct into the small intestine to aid in fat digestion. Without this vagus nerve signal, the gallbladder will remain full and not pump out the necessary bile—a condition known as obstructive cholestasis.
One of the most common surgical procedures taking place in hospitals and clinics in North America is the removal of the gallbladder, called cholecystectomy. Surgery to remove a gallbladder due to obstruction, such as gallstones, is often the first option provided to patients that begin to experience the pain associated with obstructive cholestasis. Unfortunately, most patients are not given the opportunity to determine the root cause of this condition.
Gallstones are a painful problem that can affect the gallbladder. Gallstones form in the gallbladder following a long period of low vagus nerve function, which would prevent the gallbladder from adequately pumping out bile and bile salts. When bile salts remain in the gallbladder for a long time, they begin to crystallize and form stones. This tends to happen with a lack of vagus nerve activation and is an early sign of dysfunction in this nerve. It has been shown in clinical settings that in early cases of this condition, gallstones can be released when the vagus nerve begins to function at a higher level. Performing some of the vagus nerve activation exercises and therapies that we will discuss in later chapters can be very useful for those dealing with gallbladder pain due to cholestasis and gallstone formation.
Managing Hunger and Satiety
Satiety is a medical term for having enough food during a meal. In order to be satiated, we require signals from the liver, indicating that we have enough fat, protein, and carbohydrates in the body.
When blood sugar levels rise after a meal, the small intestine releases a hormone called Glucagon-like peptide (GLP-1, for short) which communicates satiety, or fullness, to the brain, and we stop eating. Many pharmaceutical companies are now producing medications that work on the GLP-1 pathway to help manage hunger; however, this can be managed in your own body by activating the vagus nerve.
The vagus nerve offers another path to feelings of satiety. After eating a meal, vagal afferent neurons send information to the brain regarding the amount of fats that have made their way to the liver, especially triglycerides and linoleic acid. This activates vagus nerve function, sending a signal to the brain that produces a feeling of satiety and a desire to stop eating. An underactive vagus nerve may not be able to effectively send this signal, leading to continuous feelings of hunger, lack of satiety, and overeating during mealtimes. When the vagus is working effectively, it will take less than 15 to 20 minutes to feel full after a meal. If you know someone who is lacking the feeling of satiety and their hunger persists even after a large meal, they are likely suffering from vagus nerve dysfunction.
Managing Blood Sugar and Insulin Levels
Insulin resistance and type II diabetes levels are growing at exorbitant rates. Excess body weight and blood sugar control problems are major signs of health problems.
During times of stress, our bodies shift their balance toward the sympathetic nervous system and release more of the adrenal stress hormones, specifically cortisol. Cortisol increases blood sugar as part of preparing you for “fight or flight” to meet the “danger” you have imagined in your mind..
READ MORE ON STRESS AND THE BODY: https://healmindbody.com/knowledges/stress/
Under the chronic stress we experience at work and home, with our finances, relationships, friends, and families, and due to biochemical stressors and stealth infections, our bodies tend to stay in the fight-or-flight state for significantly longer than it should, and we do not shift back to the rest-and-digest state in which the parasympathetic recovery system is primarily active. The inability to shift back leads the liver to continuously produce glucose, leading to higher blood sugar levels in the longer term as well as increased insulin levels and insulin resistance.
READ MORE ON INSULIN RESISTANCE: https://healmindbody.com/what-causes-insulin-resistance/
Managing the Release of Digestive Enzymes from the Pancreas
The pancreas is not just involved in blood sugar control; it is also highly responsible for producing and secreting digestive enzymes into the small intestine in response to a meal.
When we eat, our taste buds and sensory cells in the small intestine send signals to the brain that determine the specific macronutrients that are present in the meal. Does the meal contain protein, fat, and/or carbohydrate? How much of each has entered the digestive tract, and how quickly? Once the answers to these questions are determined, the vagus signals the pancreas to release specific digestive enzymes—proteases, lipases, and amylases—to aid in the breakdown of these macronutrients, allowing for digestion and eventually the proper use of these nutrients by our cells.
In response to higher levels of protein, the pancreas secretes proteases to help break down the bonds between the amino acids that make up the proteins. In response to higher levels of fats, the pancreas secretes lipases to help break down triglycerides into cholesterol and free fatty acids. Lastly, in response to higher carbohydrate levels, amylase is secreted to help break down complex carbohydrates into simple sugars.
Without this process, our bodies would not be able to absorb the important macronutrients required for cellular function. Amino acids are mostly involved in treating new proteins within our cells, including protein and peptide hormones, neurotransmitters, receptors, and certain intracellular signaling molecules. The free fatty acids and simple sugars are used primarily for energy production, while the cholesterol component of the fats is used as the precursor to steroid hormones such as estrogen, testosterone, and cortisol.
Managing Gut Motor Function
Getting food from the mouth to the opposite end of the digestive tract is an important role of the vagus. Upon taking a bite of food, we chew that food down in our mouth until it is physically capable of being swallowed and transported through the remainder of the digestive tract.
As soon as that chewed food hits the back of the mouth—the pharynx—it is the job of the vagus nerve to push it to the next area. For this to happen, the sensors and muscles lining the digestive tract must be functioning correctly. As each bite reaches the back of the throat, it elicits a stretch reflex in the smooth muscles that signals the brainstem through the vagus nerve, letting it know where the bolus is located. In response, the vagus signals the smooth muscle cells to engage in motor activity and push the bolus of food along in a downward direction. This process is known as peristalsis.
A poorly toned vagus can be a root cause for impaired movement of a bolus through the tract. Chronic constipation and diarrhea are certainly signs of poor vagal tone and a lack of necessary activation of these muscles and nerve. Some of the biggest issues causing this problem are that we don’t chew our food well enough and that we eat in a rush and much too quickly. I call this the drive-through effect, as we are eating in a rush while in a stress-filled environment. We are trying to activate a rest-and-digest process while in a fight-or-flight state.
Basically, healthy vagal nerve transmission is required for food to move pharynx to the esophagus, through the stomach, into all three parts of the small intestine, and against gravity to the ascending and transverse colon for release from your body..
Managing the Activity of the Immune System
Just like your car needs brakes to slow down, your immune system needs to stop after activating to fight a virus or bacteria..
Without its brakes, the immune system can attack your own body, which is termed autoimmunity, or it can even stop attacking tumor cells, leading to cancer. Without brakes, a car can be a very dangerous tool. Without a system to keep it in check, the immune system can also be quite dangerous. The powerful vagus nerve is a key part of healthy immune control.
READ MORE ABOUT THE IMMUNE SYSTEM: https://healmindbody.com/knowledges/immunity/
The vagus nerve mediates the immune cells through the cholinergic anti-inflammatory pathway. When active, the pathway keeps the immune system in check and pumps the brakes when necessary. Vagus innervation to the immune organs, such as the thymus, spleen, and gut, are highly involved in activating the pathway.
The thymus is the primary lymphatic organ. It primarily produces T cells, white blood cells that seek and destroy foreign invaders. The vagus nerve sends a branch to the thymus to activate it, while sympathetic fibers that run to this organ can deactivate it. On average, the thymus is fully functional until we hit puberty, at which time it begins to shrink and decrease in both size and function. This process is called “involution of the thymus.” Recent research has shown that our high-stress lifestyle and hyperactivation of the sympathetic branches can lead to deactivation of the thymus at an earlier age. This is believed to be a root cause of autoimmune conditions and increased risk of infection by bacteria, viruses, and other invaders.
We have a higher risk of infectious disease as we get older and a higher risk of autoimmune conditions following highly stressful life events. In an autoimmune condition, our immune cells are not as well suited to distinguishing invading cells from our own cells. As we age, we are exposed to stressful life situations, and thus rates of autoimmune conditions increase, including, but certainly not limited to, Hashimoto’s thyroiditis, rheumatoid arthritis, multiple sclerosis, Crohn’s disease, ulcerative colitis, and many others.
The spleen monitors the flow of blood to control the amount of white blood cells, red blood cells and platelets. It ensures that only qualified, fully trained immune cells are present in the bloodstream and other tissues of the body. It will remove and filter out any cells that are nearing the end of their optimal functioning period. The vagus nerve relays information back and forth between the central nervous system to let our bodies know which cells are being filtered out of the blood.
As with the thymus and so many other organs, the parasympathetic activity of the vagus is required to keep the spleen active, while the sympathetic activity will temporarily decrease or shut down splenic activity. Chronic stress or activation of the sympathetic branches will undoubtedly lead to chronically decreased levels of spleen function, and in turn, poor filtration of white and red blood cells. This leads to a higher likelihood of autoimmune disease, as the roaming less-qualified “police officers” are not kept in check and are unable to distinguish between invaders and our own cellular proteins.
When a damaging event occurs in the body, or when invaders are detected, the immune cells closest to the area assess the threat and release proteins called cytokines to attract additional cells that will aid in the immune response. These cytokines are detected by vagus nerve afferent fibers that send signals back to the brain to inform it about the type of inflammation that is building up. Recent research has even shown that the vagus nerve can differentiate between cytokines.
The gut is the most common area through which invaders can enter the body, and as such, the vast majority of our immune cells are located in the lining of the gut. They are held in small pockets throughout the digestive tract, which we affectionately refer to as gut-associated lymphoid tissue (GALT). In the gut, the functions of the vagus nerve are quite extensive and necessary to ensure optimal health. It helps regulate immune and inflammatory responses, allow us to create memories, and relay information between the gut bacteria and the brain.
Managing Inflammation in the Gut
One of the most important functions of the vagus nerve is the control of immune responses in the gut via the CHOLINERGIC ANTI-INFLAMMATORY PATHWAY. Through this pathway, the vagus nerve sends signals to the cells of the immune system throughout the body, but particularly strong signals in the gut, using the neurotransmitter acetylcholine (AcH). These signals are meant to calm immune activation and decrease inflammation.
The enteric nervous system is a web of neurons embedded in the wall of the gastrointestinal tract, stretching from the esophagus right through to the rectum. It is the largest and most complex unit of the peripheral nervous system, with about 600 million neurons releasing a multitude of neurotransmitters to facilitate the motor, sensory, absorptive, and secretory functions of the gastrointestinal tract. The enteric nervous system has been called our “second brain” because so much of our health is dictated by the interaction between this system and our microbiome.
Parasympathetic activity in most of the gut is run through the vagus nerve. Its role is to keep inflammation and immune response in check. The vagus nerve and its branches send out ACh in the gut and other areas of the body to counteract the pro-inflammatory response of the sympathetic nerves and norepinephrine. When working optimally, there is a perfect balance between sympathetic NE secretion and parasympathetic ACh secretion.
Acetylcholine is released from the vagus nerve in response to higher levels of stress and immune activity.
The cholinergic anti-inflammatory pathway is a key part of vagal nerve function. This pathway plays a critical role in controlling the inflammatory response, which is an essential interface between the brain and the immune system to prevent uncontrolled immune activity which is called auto-immunity.
When inflammation of the intestine gets out of control, there is pain and altered motility, at least in part through effects on the enteric nervous system. Chron’s disease and ulcerative colitis are examples of chronic inflammatory damage.
What causes enteric nerve damage?
In addition to degenerative diseases, an immune-mediated/inflammatory response may affect both the CNS and ENS. Studies have identified that pathogenic agents, such as viruses, may disrupt or damage the integrity of the enteric neuronal microenvironment either directly or by immune-mediated injury.
Relaying Information from the Microbiome
Research into the microbiome has exploded in recent decades as it reveals the intimate and powerful relationship between the bowel ecology and our health and wellbeing. The population of bacteria in our gut is responsible for the vast majority of our nutrient health, neurotransmitters, our mood, and even how our brains work.
There are nearly 100 trillion bacterial cells in our digestive tract, which is more than the total number of cells in our body. This natural ecological balance of these bacteria can affect nearly every aspect of our health and well-being. The vagus nerve is the neurological highway that provides communication between the life supporting gut bacteria and our brains. Cytokines and hormones circulating in the blood are also part of this essential alliance.
Food craving is an example of this powerful gut-brain connection. According to The Psychobiotic Revolution, written by Scott Anderson, John Cryan, and Ted Dinan, “Your cravings are often just committee memos sent up from your gut microbes. They contain a complete list of the carbs, sugars, and fats they are looking for.”
The book continues to discuss the example of Bifidobacterium (a.k.a. Bifido), a genus of bacteria that is found in high proportion in our gut: “Some microbes, especially our friendly Bifido species, produce butyrate, which feeds and heals the lining of your gut. Butyrate can make its way to the brain, where it can induce a good mood, dampen inflammation, or encourage the production of a brain-growth hormone. All these changes can improve your mood and even help you think better.”
Another type of bacteria that is discussed in this book are in the Lactobacillus (a.k.a. Lacto) genus. Anderson, Cryan, and Dinan elaborate: “In studies with people suffering from IBS, it was found that some Lacto species actually manipulate the opioid and cannabinoid receptors in the brain, acting almost like a shot of morphine. Like the addiction to a runner’s high, this kind of reaction can lead to cravings for whatever food your Lacto microbes prefer. You might think your cravings are all in your mind, but chances are they begin with the bacteria in your gut.”
Once we realize that cravings and signals regarding the foods our bacteria want are actually being relayed by the vagus nerve and through our bloodstream, it is possible to take back control of our choices and make dietary changes that can have a beneficial effect on our microbiome and our overall health.
Allowing Us to Create Memories
Recent research has shown that the presence of gut bacteria is necessary for development and maturation of the enteric nervous system as well as the central nervous system. As discussed earlier, the vagus nerve is highly involved in the relay of microbiome information from the gut bacteria to the brain. This chain of communication may be responsible for activating production of a protein called brain-derived neurotrophic factor (BDNF). Activation of BDNF leads to increased neuronal connectivity, and most importantly, the production of memories in the brain.
This means that without gut bacteria and a healthy functioning vagus nerve, it may be difficult to form new memories and create new neuronal connections. To an even greater extent, this means that if you have an optimally functioning vagus nerve, you will likely be able to form greater memories and associations with the world around you and those who are important to you.
During our fetal development, we produce barriers to protect us from external threats. The gut-blood barrier is one such barrier, protecting us from bacteria (both good and bad) that may want to invade. It is formed from the same cells that produce our blood-brain barrier. This means that any inflammation that occurs in the gut and causes the gut barrier to break down also has the ability to break down the blood-brain barrier.
“Brain fog” is a common medical complaint and is the result of higher levels of inflammation in the brain. Brain fog occurs when the blood-brain barrier has broken down slightly and inflammatory signals are allowed to enter the brain tissue, decreasing the function of neurons.
In other words, brain fog is due to defects in the blood-brain barrier and inflammation in the brain, which is due to increased bowel wall permeability, or “leaky gut”.





