ACTIVATE YOUR VAGUS NERVE – UNLEASH YOUR BODY’S NATURAL ABILITY TO HEAL
Gut Sensitivities, Inflammation, Brain Fog, Autoimmunity, Anxiety, Depression written by Dr. Navaz Habib, Ulyssess Press, Berkely California, 2019
Summary written by Ronald Peters MD, MPH, MindBody Medicine Center
PART 3: WHAT COULD GO WRONG WITH THE VAGUS?
PART 4: HOW DO YOU MEASURE AND ACTIVATE THE VAGUS?
PART 3: WHAT COULD GO WRONG WITH THE VAGUS?
VAGAL NERVE DAMAGE AND RECEPTOR DAMAGE IN ORGANS
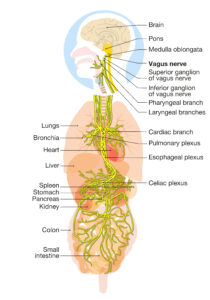
Approximately 80 percent of the signals being sent along the vagus are in-coming from the organs to the brain—afferent signals. The vagus, which is the longest nerve in the body, receives communications information from the liver about detoxification, bile production, and blood sugar balance; from the digestive tract about the digestive process, movement of food, and the microbiome; and most importantly, from the immune system cells and organs about their state of function. It also relays information from the heart and lungs regarding their activity levels and any impairments that are taking place.
 The vagus nerve is protected by Schwann cells that create an insulating barrier around the nerve which is called a myelin sheath that protects signals and ensures nerves function effectively. Any damage to these Schwann cells can lead to “fraying” of the insulation and ineffective signaling along the nerve.
The vagus nerve is protected by Schwann cells that create an insulating barrier around the nerve which is called a myelin sheath that protects signals and ensures nerves function effectively. Any damage to these Schwann cells can lead to “fraying” of the insulation and ineffective signaling along the nerve.
Once an electrical signal reaches the end of a neuron at the area called the terminal axon, the signal creates a charge that induces a neurotransmitter to be released from the cell. There are many different neurotransmitters in the body, such as epinephrine, norepinephrine, and serotonin. The vagus nerve almost exclusively uses a neurotransmitter called acetylcholine, or ACh for short.
Acetylcholine is biochemically created from acetyl coenzyme A (acetyl-CoA) and choline. Through different metabolic processes, glucose and free fatty acids are broken down into acetyl-CoA. These metabolic reactions require specific micronutrients to function optimally. To metabolize free fatty acids, our cells require sufficient amounts of carnitine and vitamin B2, while to metabolize glucose, our cells require high quantities of vitamin B1, vitamin B3, chromium, lipoic acid, and coenzyme Q10.
Unfortunately, many people are deficient in one or more of these key nutrients. Lab testing can identify nutrient levels, such as the Organic Acid Test.
Choline, on the other hand, is an organic compound that comes from certain amino acids. It is considered an essential nutrient for humans, meaning it cannot be produced within our body—it must be taken in as part of the diet. The foods that contain this compound in the highest quantities are eggs and other animal products as well as many plant-based foods, such as soy, potatoes, beans, wheat germ, brown rice, broccoli, cabbage and more.
The vagus releases acetylcholine which binds to receptor proteins on the surface of many types of cells throughout the body thus activating a specific biological response.
About 50% of bacteria in the gut are termed “gram negative” and they have lipopolysaccharides in the cell wall to provide structural integrity and a barrier to protect the cell from toxins and bile salts. However, LPS molecules activate the immune system and the release of messenger cytokines, or messenger molecules, which can lead to inflammation and even fever.
Lipopolysaccharides can also damage or decrease the receptor cells on organs connected to the vagus. In the presence of LPS, the gene that holds the blueprint for this receptor protein has the potential to become significantly more or significantly less active. This can explain why some people are highly sensitive to inflammatory gut changes and some are less sensitive. Regardless of sensitivity levels, LPS is a trigger for changes to this gene and causes issues for receptor protein concentrations.
DYSFUNCTIONAL BREATHING
The first and most common cause of vagal nerve dysfunctional signaling in the vagus nerve is unhealthy breathing.
As a baby, we learn to breathe in the automatic and correct way. The next time you are around a healthy infant or toddler, take a moment and watch how they breathe. What you will notice is that for them to take a breath in, their diaphragm must contract, and in doing so, they will expand their belly in the process. Diaphragmatic breathing is the process of using this major muscle rather than accessory muscles for breathing.
This natural and healthy breathing is gradually lost under the many stresses of modern living, and we begin learning to breathe in a different way. We start to use our accessory muscles for breathing—the backup muscles that are more important and useful during stressful situations. We begin to control the expansion of the thorax and creation of the vacuum using the muscles of the neck, shoulders, and upper, mid, and lower back, as well as the anterior chest muscles.
We have been chronically training ourselves to breathe incorrectly and inefficiently for years for the superficial reasons that have been subconsciously ingrained in each of us from early in our lives. This has led to issues in multiple nerves. The phrenic nerve has not been trained to breathe correctly, as we don’t generally use our diaphragms to breathe with our bellies. In the same respect, as we are not fully expanding and creating effective vacuum effects, the lungs are not expanding effectively, and the vagus nerve signals as such. Vagus nerve signaling becomes less efficient as our breathing becomes less effective.
Breathing is the first act of life, and the last. Our very life depends on it. Since we cannot live without breathing it is tragically deplorable to contemplate the millions and millions who have never mastered the art of correct breathing.
—Joseph Pilates
Learning to breathe correctly is one of the simplest and best things you can do for your health. Proper breathing techniques are at the root of so many different therapies, practices, and trainings.
Another symptom of incorrect breathing patterns is the inability to control stress. Those who feel chronically overwhelmed by emotional and physical stressors often have very poor breathing habits. The next time you get riled up or find yourself in an argument or heated discussion, pause and take a moment to consider your breathing. In these situations, we usually take short and shallow breaths, which activates our fight-or-flight response. Pausing and taking deep breaths helps us become more rational and calm, which helps us create a positive resolution very quickly. Those with poor vagal tone tend not to be able to control their anger, so they will often lash out quickly and raise their voice, altering their breathing patterns toward these shallower and quicker breaths.
Dysfunctional Airways
“Allergies” are most often associated with allergic rhinitis with stuffy or drippy nose and sinuses. Obviously, if your airways are not clear, it is difficult to breathe in deeply and fully. This can be a constant issue for someone dealing with a deviated septum, chronic adenoid inflammation, and post-nasal drip. All these issues can lead to the airways not functioning optimally. The nasal passage, the pharynx, the larynx, and the trachea—together, these are known as the upper respiratory tract. There are a few different insults and issues that can affect our airways negatively and I will discuss each one in this section. The first is dysfunctional posture.
We live in the smartphone and laptop age. We sit at our desks and stare at our computer screens for hours on end, then take breaks from our computers to look down at our smartphones. We spend hours in a poor posture, leading to back and neck pain, then hold our cellphones below our chin. For the most part, we are all aware that postural issues contribute to neck, back, and shoulder pain and mechanical dysfunction of the spine, but it’s easy to forget the problems that it causes with airways and the ability to breathe correctly.
Here’s another test for you to do right now.
I want you to sit in a slouched position and try to take a deep breath in by expanding your belly—breathe with your diaphragm.
Another issue when we are looking down at our laptop screens is that our necks are flexed forward for long periods of time. This position constricts our airways, so the muscles of the pharynx and larynx are unable to remain tight and allow the airway to stay as open as possible.
Snoring and sleep apnea are major health issues and far more common than most people can imagine. Approximately 44% of men and 24% of women snore while asleep. The tongue is too large for the mouth and during the night it partially obstructs the airway. If the airway is fully blocked, we awaken in a startle, which is called sleep apnea. Sleep apnea is diagnosed with a sleep study.
READ MORE ON THE MEDICAL CONSEQUNCES OF SLEEP APNEA
https://healmindbody.com/leading-causes-of-death-rooted-in-a-structurally-impaired-mouth/
We are meant to breathe through our nose; the mouth is simply a backup plan. After all, our noses have hairs to filter the air, and our mouths have teeth to chew food. Speak to any dentist and they will tell you that without a doubt, the patients who breathe through their mouths have significantly greater oral health concerns than nose breathers. Mouth breathing dries out the saliva and can be considered dangerous. A dry mouth allows bacteria to grow unchecked by antibodies in our saliva, which leads to bad breath (halitosis), tooth decay, and cavities. This issue is also often accompanied by chronic nasal passage obstruction. A lack of airflow through the nasal passage leads to chronic sinus infections and post-nasal drip.
Training yourself to breathe through your nose is possible and will be discussed in greater detail in the next section. It is also important to train the muscles of the pharynx and larynx to increase muscle tone and vagal tone.
Monotone Voice
A patient suffering from much emotional stress recently came to my office. She had gone through a tough breakup and had some trouble at home with her parents. She was dealing with a diagnosis of irritable bowel syndrome and had been prescribed multiple medications to help manage these symptoms, but with very minimal changes to report from them. One of the signs that I noticed during our initial assessment was that she was not fully capable of increasing and decreasing the pitch and tone of her voice. Her voice was quite monotonous.
Monotony is a sign of poor control over the laryngeal muscles, which manage the tension levels of the vocal cords. When someone has a monotone voice, it is a sign that signals are not effectively passing through the motor component of the vagus, thus the muscles are not receiving enough signaling to tense, lengthen, relax, or stretch the vocal cords. This leads to very slight change in the tension of the cords, and thus, inability to control pitch or tone of voice.
I immediately recommended some specific vagus nerve toning exercises to this patient, and in just two months, she was able to notice significant changes in her health and in the tone of her voice. She was able to have greater control of her speech and had improved communication levels with her parents. If you listen closely to yourself or those around you, it is possible to pick up on these small signs that can point you in the right direction.
DYSFUNCTIONAL DIGESTION
Have you been told that you eat too quickly? Have you ever counted the number of times you chew your food with each bite? Next time you eat, take a moment and actually count the number of times you chew each bite of food and how long you sit down for your meal.
You may be wondering, “Why does this even matter or make a difference in vagus nerve signaling and your overall health?” Well, the answer is complex, but it makes a lot of sense when you understand the importance of digestive sequencing.
When you get hungry, your brain receives signals from your gut bacteria and from cells in your body, asking to be fed with the required nutrients to create energy and build up reserves for future needs. Each of your cells requires macronutrients. Fat and carbohydrates are needed for energy production, and dietary protein and its component amino acids are needed for internal protein production. Each of the processes inside of our cells also require vitamins and minerals to allow these functions to occur. All nutrients enter your body through the digestive tract —but only if the sequence of digestion is adhered to.
An optimal digestive sequence takes approximately 16 to 20 hours to complete, from ingestion of food to release of waste products. There is quite a bit of variation between people, male and female, healthy and unhealthy, but a transit time shorter than 10 hours is considered too fast, while longer than 24 hours is considered too slow. Diarrhea and constipation are very common concerns that 20 to 40 percent of people deal with at any given time. As vagus nerve activation is responsible for digestive sequencing and peristalsis, dysfunctional digestive rhythm is directly correlated to vagus nerve dysfunction.
If digestion occurs too quickly (i.e., in less than 10 hours), you are likely dealing with a lack of nutrient absorption, while digestion taking longer than 24 hours is associated with increased toxin build-up, a rise in opportunistic bacteria, and leaky gut. A longer transit time within the optimal period (16 to 20 hours) is strongly correlated to greater microbial diversity— a healthier and more diverse population of bacteria in the large intestine. Once your gut bacteria and internal cells decide that they are hungry or in need of nutrients, they send a signal up the vagus nerve to the brain, promoting you to feel the hunger. You are sent to pick up your next snack or meal by the signals sent from your microbiome.
Chewing your food adequately is very important. Your mouth is the only place along the entire digestive tract that has teeth, so is the only place that can physically break down your bite. If you do not chew each bite well enough, then you will not break the food down into small enough morsels to activate the taste buds on your tongue and mouth. The taste of each bite is signaled to the brain to determine how much protein, fat, and carbohydrates are present. Then, the vagus nerve signals the stomach, liver, gallbladder, and pancreas to create and pump out the correct amounts of stomach acid, bile, and digestive enzymes. Poor vagus nerve signaling contributes to malnutrition, but this is often overlooked.
Eating quickly and not chewing well contributes to a lower level of satiety, higher caloric intake, poorer food choices, and malnutrition.
After chewing, the vagus signals the pharynx and larynx to allow the chewed bite to enter the esophagus and be pushed down to the stomach using peristalsis. Once the food reaches the stomach, stomach acid breaks it down into macronutrients and in digestible fiber. The stomach then continues to churn and push it into the first part of the small intestine. In this location, the liver, gallbladder, and pancreas release their enzymes and bile to help further break down and absorb nutrients into the bloodstream. Upon being absorbed in the bloodstream, fats, carbs, and amino acids are transported to the liver for filtration first, then throughout the rest of the body to be used by the cells for energy production and protein building.
The vagus nerve facilitates movement of the indigestible fiber through the small intestine and ileocecal valve to reach the proximal colon of the large intestine. Here, the large bacterial population breaks down the fiber (which we are unable to process with our digestive enzymes) into vitamins, minerals, and precursors for hormones and neurotransmitters.
The entire digestive sequence is primarily controlled by the vagus nerve and this key regulatory process is easily disrupted by emotional stress. Along with strong immunity and hormone production, digestion is a parasympathetic process which is quickly turned off by stress, which is a sympathetic function designed for survival. The sympathetic nervous system is designed to prepare us for “fight or flight.”
When we grab a quick meal while running out the door in the morning, we are eating in a stressed situation. When we eat our lunches in front of our work computers, we are eating in a stressed environment. When we don’t pay attention to the food in front of us, we are unable to send the correct signals to our brain and digestive organs to get the digestive process functioning optimally. Even our dietary choices affect this process and the nerve that controls it.
To optimize digestive sequencing and vagus signaling to and from the digestive tract, it is necessary to eat in a low-stress state of mind. This means taking time to sit down and eating each meal in a relaxed location. If you are at work, go sit outside or at least away from your desk. If you are in a rush, take a cup of coffee or tea rather than food on the go.. Create relaxed, restful environments where you can sit comfortably and eat your meals, so you are not beginning the digestive sequence in a stressed state.
Bacterial Overgrowth and Vagus Dysfunction
Small intestinal bacterial overgrowth, SIBO, is a common cause of digestive distress. It occurs when the bacteria that should only be in the large intestine overgrow and spread into the small intestine, moving in a backward direction. It is a common cause of irritable bowel syndrome, Crohn’s disease, and ulcerative colitis. SIBO is often associated with other autoimmune conditions. If SIBO is not taken care of with basic herbal and supplement protocols, it can become recurrent.
Vagus activation is necessary to push food forward along the intestinal tract in one direction. If bacteria are moving in the opposite direction, this leads us to understand that there is a weak signal being sent through the vagus that allows this motion to occur. This can happen at the ileocecal valve itself (the valve that stops food from going back from the large intestine into the small intestine) or throughout the digestive tract. For this reason, recurrent SIBO is a common finding when vagus nerve is weak and needs to be activated.
Dysfunctional Dietary Choices
Poor dietary choices can lead to ineffective vagus signaling, dysfunctional digestion, and nutrient deficiencies that affect each cell in the body. Regardless of what diet you choose to follow, some food choices negatively affect our health and are understood to cause issues for a vast majority of people.
Highly processed foods made of low-quality ingredients are the major culprit in this battle. Most of these foods are found within the aisles of your grocery store. They are the “food products” sitting in boxes and bags in the center of the store, with shelf-lives longer than any of their individual ingredients would last. Foods containing emulsifiers and preservatives to increase their shelf-lives have a direct correlation with increased levels of inflammation and gut microbiome changes toward dysbiosis.
Most food products with more than four ingredients listed on the package are likely to be poor options. This includes crackers, breakfast cereals, beverages with added sugar or sweeteners, etc. Low-fat, high-sugar diet foods that claim to be low in calories are often also low in the nutrients your bacteria want and your cells need. Fast food and pre-prepared meals are generally made using low-quality ingredients, which have been shown to increase inflammation and negatively change bacterial populations.
These choices trigger opportunistic bacteria to grow and produce higher amounts of toxins, most commonly LPS, which are known to break down the bonds between the cells of the intestinal tract and enter the bloodstream. This molecule has negative effects on many of our cells, including brain and liver cells. LPS is used by researchers around the world to simulate and produce inflammation in their subjects for testing. In high quantities, it produces a life-threatening situation called sepsis, but in chronic exposure to low quantities, as seen in a dysfunctional gut, LPS triggers chronic low-grade inflammation.
Research shows that activation of the vagus nerve reduces the inflammation triggered by LPS. Problems occur as stress levels increase and vagus nerve signaling becomes dysfunctional. This allows LPS to wreak havoc on your gut lining and have far-reaching effects on your immune system, leading to autoimmune disease, metabolic diseases, and even cancers.
Food choices can reverse LPS-led inflammation and help improve the function of the brain, nerves, and even the vagus itself. By volume, the brain is made up of more fat than any other component. The brain and nerves are insulated by fat to ensure their function. The good fats in our diet can improve the insulation around these nerves and trigger proper signaling within the vagus nerve itself. When we take in high-quality, minimally processed dietary fats, our intestines and gut bacteria send a signal of CCK to the enteric nerves and then to the vagus. This activates vagus function and leads to activation of the cholinergic anti-inflammatory pathway.
As stated by Michael Pollan, the author of the book In Defense of Food, the summary is “Eat food, not too much, mostly plants.” I take this to mean the following:
- Eat real food: Whole grains, vegetables, fruit, high quality seafood and minimize meats
- Not too much: If you eat slowly, you can enjoy each bite and feel fuller while eating less overall.
- Mostly plants: About 75 percent of what you eat should grow in or on a plant. Fruits and vegetables are generally unprocessed, contain the vast majority of the nutrients that your body needs, and often taste
- significantly better than you realize.
Chemicals on Our Foods
Do you choose organic options whenever possible? If not, you should certainly consider it, if not make it an absolute priority. If you have not heard, the effects of herbicides and pesticides on our health can be significant and have much farther-reaching effects than anyone ever anticipated.
Glyphosate is the main culprit here. It is the most widely used herbicide on earth, affecting many of our agricultural crops. The herbicide kills off weeds without actually killing the crop it is sprayed on. Crops such as corn, soy, canola, cotton, alfalfa, and sugar beets are genetically modified to not be affected by the glyphosate molecule. But the glyphosate depletes these crops of a very important micronutrient called manganese, which is required for many functions in our bodies.
READ MORE ON GLYPHOSATE:
https://healmindbody.com/weeding-out-vaccine-toxins-mmr-glyphosate-and-the-health-of-a-generation-2/
Poor Satiety Reflex
I used to have a lot of trouble regulating the amount of food that I ate. I was unable to notice when I felt full near the end of a meal, so I would simply eat and eat. The neurological reflex from my stomach was very slow, and this resulted in my overeating at each meal, as well as having many snacks. This is what led me to become significantly overweight and was the root of my health conditions prior to finding functional medicine.
A poor satiety reflex is one of the most common signs of an impaired vagus nerve in North America today. As we are aware, the obesity epidemic is growing at unprecedented rates. This leads to heart disease, diabetes, and soaring cancer rates. Many of these conditions are preceded by signs of vagus nerve dysfunction, and a poor satiety reflex is one of the most common signs. Whether they recognize it as vagus dysfunction is an entirely different question.
The vagus nerve innervates the stomach and sends information back to the brain regarding the amount the stomach has stretched. Often, it takes time to have this signal completely optimized, and those of us with less than optimal vagus nerve function tend to have an even slower reflex. The inability to feel full or satiated near the end of a meal is a sign that the vagus is not able to send these signals. This issue is exacerbated by the fact that we are living in the fast-food era and eating under stressful circumstances. When we do not take the time to rest and digest in the parasympathetic state, it is nearly impossible for us to regulate our food intake, and thus, the vagus nerve is not being exercised and trained to let us know when to stop eating.
Take a moment and think about your stress levels during your last five or six meals. Were you eating in a relaxed environment or at your desk in front of your computer? Were you enjoying a good laugh with loved ones, or were you rushing through the drive-through while trying to make it to an important meeting? The environment in which you eat determines the ability to train your vagus nerve to send these signals to your brain.
DYSFUNCTIONAL MICROBIOME
One of the most likely low-grade stressors that you may not be aware of is the bacteria living in and around you. The population of bacteria living in your gut and on your skin has a significant effect on us, and if that population is not balanced; it can be a major stressor on your body.
There are approximately 100 trillion bacteria present in our large intestine alone, compared with the 40 to 60 trillion human cells that make up our body. There are even some estimates that state there are 10 times more bacterial cells living in and on us than there are human cells in our bodies. Interestingly, there are 150 times as many genes in our microbiomes than there are in the human genome. It has also been proven that the composition of our microbiomes has a direct relationship to our diet and health as we age.
All disease begins in the gut.
—Hippocrates
As we know, the vagus nerve is highly involved in signaling to and from the small and large intestines. It signals the digestive tract to activate smooth muscle cells, allowing these muscles to contract. This activates peristalsis following a meal and something called the migrating motor complex between meals. The VN also sends anti-inflammatory signals to the immune cells, ensuring that the system keeps the brakes on as necessary. Information is also relayed from the gut bacteria to the cells of the digestive tract, which then sends signals to the central nervous system via the vagus nerve.
READ MORE ON THE MICROBIOME
https://healmindbody.com/the-gut-microbiome-the-invisible-ecosystem-integral-to-your-health/
The Effect of Stress on Gut-Brain Function
The bacterial population is very important in dictating health and we have learned much about its effects over the last decade. Although we are still unclear about how the vagus nerve communicates with the microbiome and which vagal afferents are activated by which gut bacteria, there is much research to show that many of the effects of the gut microbiota on brain function are highly dependent on vagal activation and its specific signaling. The byproducts of bacterial metabolism include very important and nourishing molecules called short-chain fatty acids (SCFAs), which are important in reducing the amount of inflammation in the gut and throughout the body. Butyrate is the most-researched SCFA that has shown to be lacking in those with high levels of inflammation.
Here is what they found as stated by Paul O’Toole and Ian B. Jeffery in “Gut Microbiota and Aging” published in the journal Science, “Although not significantly associated with chronological aging, loss of diversity in the core microbiota groups is associated with increased frailty.” This essentially means that as we lose microbiome diversity and representation from various groups of bacterial populations, our health suffers, leading to decreased strength and cognitive performance. What we are fed both early and later in life can dictate this population and set us on a path of health or disease. The excessive use of antibiotics early in life can significantly skew the microbiome diversity and increase our risk of disease later in life by decreasing the Firmicutes bacteria levels and essentially eliminating Actinobacteria levels. When we have an imbalanced bacterial flora and low microbiome diversity, our levels of SCFAs like butyrate actually decrease, increasing our risk for inflammatory health conditions.
Preliminary studies in mice have shown that the vagus nerve is activated by vagus signaling from specific species of bacteria. A study published in the Proceedings of the National Academy of Sciences showed that Lactobacillus rhamnosus affected GABA levels in different parts of the brain, improving stress levels and cognition. Notably, this only occurred when subjects had an intact vagus nerve. The researchers suggest these bacterial interactions could be an option for treating anxiety and depression. Another study showed that exposure to Bifidobacterium longum can decrease levels of anxiety-like behavior in mice with colitis. The effect was significantly faster and more efficient in mice with an intact vagus nerve. On the other hand, Campylobacter jejuni infections can increase anxiety like behavior—which is linked to inflammation—according to a 2008 study published in Brain, Behavior, and Immunity. These reactions were likely activated via the vagal pathway.
Although they make up the vast majority of the microbiome, bacteria are not its only members. It’s also important to keep in mind that we may also have viruses, fungi, protozoan parasites, and worms living in our digestive tracts, contributing to the levels of inflammation in our gut. Indeed, there are many parasites that can have functionally detrimental effects on the function of your gut and the signaling to and from the vagus nerve. A 2015 review by Halliez et al. published in Frontiers in Cellular Neuroscience described the effects of certain parasites on the gut: Cryptosporidium parvum infections can lead to decreased nutrient absorption due to the parasites breaking down the cells of the gut lining. Abdominal pain is a symptom of a C. parvum infection. Giardia duodenalis is a parasite that alters gut motility, which has a direct effect on vagus nerve, and prevents nutrient absorption through the breakdown of gut lining cells. Additionally, G. duodenalis has a negative impact on the cells in the gut that help produce serotonin, thus potentially reducing serotonin levels. Serotonin is important for signaling from EECs to the vagus nerve as well as regulating your mood. A final example is Entamoeba histolytica, which alters cellular function, including electrolyte transportation, secretion, and malabsorption of nutrients, thus affecting the function of all cells, including those of the enteric nervous system, which lea ds to a direct signaling breakdown to the vagus nerve.
Viruses are also possible causes of nerve dysfunction, as they can enter the body through the gut. There is a very likely hypothesis that viral infection of the vagus nerve itself may contribute to chronic fatigue syndrome. There is a real correlation between poor vagus nerve activity and the symptoms of chronic fatigue syndrome, which include fatigue, sleep changes, loss of appetite, depression, malaise, and cognitive impairment, as well as clinical signs of inflammation and an inability to decrease inflammation.
You can, however, be tested for most of these good and bad members of your microbiome. In my practice, we use a functional stool test called the GI-MAP test from Diagnostic Solutions Laboratory, which uses DNA-PCR technology to identify the specific species of bacteria, parasites, viruses, and fungi that are living in your gut. Using this information, we can determine the correct next steps for eliminating these blind spots that are likely causing significant health issues in those who are dealing with them.
CHRONIC INFLAMMATIOND AND IMMUNE ACTIVATION
Chronic inflammation is the most common and obvious sign of ineffective signaling from the vagus nerve. It is unfortunately overlooked by many health care practitioners. Once we are able to test for, determine, and eliminate the root cause of the inflammatory response, inflammation levels should come down. Very commonly, however, these levels do not drop as easily as we would like.
Chronic inflammation can show its face in different ways, from low-grade arthritis-type pain in the knees, ankles, hips, shoulders, and wrists to unmanaged autoimmune conditions that destroy cells without our realizing what they are doing. If the vagus nerve is functioning optimally and can send signals to shut down inflammation levels, then once the cause of the condition has been eliminated, vagus signaling should be able to reduce these levels on its own. Improving vagal tone can help reduce these inflammatory signals and limit the amount of damage they can have on function and structure.
If someone is suffering from chronic inflammation levels that have persisted for months and even years, the first step is to determine and deal with the root cause. As we have discussed, many of our immune and inflammatory cells are housed in the gut. Testing the gut to confirm that there are no inflammatory triggers is the best way to deal with the root cause of inflammation. While dealing with these triggers, vagus nerve tone will help limit the damage, so performing exercises to improve signaling will work effectively to manage inflammatory levels.
Autoimmune Conditions
Autoimmunity is the fastest growing health condition in North America due to our lifestyles, chronic stress, unhealthy diets, and lack of understanding of the true cause of these conditions. I have worked one-on-one with hundreds of patients who have been diagnosed with autoimmune diseases such as type 1 diabetes, multiple sclerosis, Hashimoto’s thyroiditis, psoriasis, rheumatoid arthritis, Graves’ disease, Crohn’s disease, systemic lupus erythematosus, celiac disease, alopecia areata, and many others. The one commonality I have come across is that my patients have not been informed of how the condition started in the first place.
As we now know, the largest volume of our immune cells are located in the gut, in areas of the intestine called gut-associated lymphatic tissue, or GALT. This is where much of our primary immune responses take place, as the digestive tract is quite sensitive to penetration from invaders and toxins. These invaders and toxins are triggers for immune cells to become active, and in some cases, overly active.
Although genetics plays a role in the risk of developing an autoimmune condition, genes are simply a blueprint. The array of environmental triggers are the major reason why these conditions start in the first place. In fact, there is much research showing that genetics determine only one-third of risk of disease development, while non-genetic environmental and triggering factors contribute the remaining two-thirds of the risk.
Chronic Inflammation of the Gut
The stool test that I use in my office (GI-MAP DNA stool analysis from Diagnostic Solutions Laboratory) is great at telling us exactly what is living there—any potential autoimmune-triggering bacteria that send out these high inflammatory signals, as well as the current level of immune system function and the amount of inflammation in the gut.
As we are aware, the effect of the vagus nerve is to slow the level of inflammation and keep it in check. If we are sending repeated messages of inflammation over a long time, we are essentially training the vagus nerve to stop having its positive anti-inflammatory effect. This is why it is most common for people to begin experiencing and receiving diagnoses of these autoimmune conditions in their 30s and 40s. After 30+ years of inflammatory signals, the vagus nerve has been trained to stop functioning as an anti-inflammatory intervention. Between the ages of 35 and 40, the vagus tone has decreased significantly and the anti-inflammatory signals stop being sent out. These conditions often arise following the stress of pregnancy, having children, and lacking sleep during the first years of a child’s life—all of which are stressors that decrease vagus nerve function.
Inflammation Due to Physical and Emotional Trauma
Inflammation is a protective mechanism that occurs in our bodies to protect us from damage; it does not only increase in response to biochemical signals from the gut. When a child bumps their head or falls down, they may develop swelling or a bruise in a localized area, which is actually a collection of cells and cell signals working to repair any damaged tissue. Problems tend to occur when signals for inflammation take place over a longer timeline. Inflammation levels are good for the body, but only if they are kept in check by the vagus nerve and the cholinergic anti-inflammatory pathway.
Repetitive signals for inflammation due to physical trauma can occur for various reasons—multiple automobile accidents, multiple pregnancies, repetitive strain injuries, improper weight-lifting technique, and weaker muscles are all possible sources of chronic physical injury and inflammatory signaling.
Emotional trauma can include stressful life events that create a negative impact on mind and body. Life events such as the passing of a loved one, the loss of one’s job or income, emotional and mental abuse, or the emotional burden of a severe physical injury impacting independence are common and seen by functional medicine doctors like myself quite commonly in practice. Traumatic life events activate the sympathetic nervous system, preparing us for “fight-or-flight”, which includes increasing the inflammatory process.
READ MORE ON THE POWERFUL INFLUENCE OF STRESS ON MIND AND BODY
https://healmindbody.com/knowledges/stress/
DYSFUNCTIONAL HEART RATE
Electrical signals from the vagus nerve and sympathetic nerves dictate change to the heart rate. The lower your resting heart rate, the stronger your vagus nerve. Interestingly, there are studies suggesting that one’s lifespan is inversely correlated to resting heart rate—thus, the lower your heart rate, the longer you will live. From this, we can extrapolate that stronger vagus nerve tone and function is associated with lower heart rate and thus a longer natural life expectancy.
When a car goes spinning out of control on an icy road, the driver will immediately feel stressed and enter the fight-or-flight state. The sympathetic nerves activate instantly and the vagus is shut down. The signals from the sympathetic nerves speed up the heart rate by signaling that the muscles of the arms and legs need much more oxygenated blood to control the steering wheel and push on the brakes of the car. Once the car comes to a safe stop, the sympathetic nerves slowly stop firing and the vagus activates to slow the heart rate using calming, rhythmic electrical signaling.
One sign of a dysfunctional vagus nerve is the inability to quickly normalize the heart rate after this type of stressful event. The amount of time a person spends with a high heart rate and shallow breathing following a stressful occurrence is a strong sign of vagus nerve function. One who can quickly calm their nerves and slow their heart rate has a very strong vagus nerve, while someone who takes longer to come back to their resting rate is likely suffering from dysfunctional vagus nerve tone. How well do you function under the pressure of a high-stress situation like this? Do you remain very calm and rational when dealing with such a scenario?
In addition to an underactive vagus, the nerve can be hyperactive. Vasovagal syncope is a major issue caused by underactive sympathetic nerves and hyperactive vagus nerve. Syncope is the medical term for fainting. The sympathetic nervous system acts to increase heart rate and blood pressure while the parasympathetic nerves act on the heart to slow heart rate and decrease blood pressure. If the sympathetic nerves are weak and the vagus nerves are overactive, the result is a temporary loss of consciousness that is not life-threatening.
Vasovagal syncope is a sign of improper balance within the autonomic nervous system. It is a common concern without a single clear cause. In fact, there are many different causes, and the mechanisms are very different between younger and older individuals.
The inability to regulate the autonomic nervous system is called dysautonomia. The mechanisms that lead to dysautonomia can be genetic, as with Charcot-Marie-Tooth disease and Ehlers-Danlos syndrome, or they can physically manifest, as with pregnancy, physical trauma, Chiari malformations, or surgery. The most common causes, however, are related to immune and metabolic health conditions. When the cells of the nervous system lack the correct nutrients for healthy metabolic responses or are dealing with high levels of toxicity, the nerves are not able to function quickly enough. Even more of a concern are autoimmune conditions that affect the nerves themselves, as well as the organs innervated by the VN and the sympathetics. These conditions include Parkinson’s disease, sarcoidosis, Crohn’s disease, ulcerative colitis, Sjogren’s syndrome, amyloidosis, and even chronic inflammatory demyelinating polyneuropathy.
When someone deals with an issue like vasovagal syncope and has relatively common fainting spells, it is often a sign of an immune or metabolic issue that may not yet be diagnosed. Functional lab testing and functional neurology provide insights to the potential underlying root causes of this issue, which is often a symptom of improperly functioning nerves in the autonomic nervous system and hyperactivation of the vagus. Changes in heart rate, blood pressure, and cardiac output that cannot be fully regulated are signs that vagus and the autonomic nervous system are not functioning optimally.
LIVER DYSFUNCTION
Your liver performs hundreds of tasks every second. From continuously sensing and managing blood sugar to filtering toxins from the blood to producing bile salts, the effects are far-reaching and affect the entire body. The liver requires a certain set of nutrients to do its job optimally.
One of the liver’s jobs is to detoxify the blood, essentially filtering out any hormones, neurotransmitters, drugs, and toxins that should not be present in high quantities. Toxins can be produced inside the body as end products of metabolism or as endotoxins, which are released by bacteria and cross into the bloodstream. They can also be exotoxins such as drugs, agricultural chemicals, food additives, household chemicals, and pollutants. These toxins can be either fat soluble or water soluble. The liver has a two-stage filtering process that it uses to clear all of these potentially harmful substances out of the blood.
In the first phase of detoxification, five different types of reactions occur so the fat-soluble toxins can become less fat soluble. These reactions require many B vitamins (specifically B2, B3, B6, and B12), folate, glutathione (one of the strongest antioxidants in the body), branched-chain amino acids, flavonoids, and phospholipids. Many of the patients that come to see me are deficient in most of these nutrients, either because their diets are lacking these nutrients, or because their digestive processes are not effectively getting these nutrients into the body.
Once the liver completes the first stage, the toxic substances tend to be highly reactive and are a risk to the health of our cells. These highly reactive substances are called reactive oxygen species, and we need a strong set of functioning antioxidants to counter any damage they may do to our cell surfaces and even our DNA. These antioxidants include vitamins A, C, and E, coenzyme Q10, thiols, selenium, copper, bioflavonoids, zinc, silymarin, manganese, and pycnogenol.
If the liver has enough nutrients (including many of those required for phase one), these reactive oxygen species undergo the six reactions of phase two to become entirely water soluble. One of the reactions is called amino acid conjugation, and it requires certain amino acids—N-acetylcysteine, glycine, taurine, glutamine, cysteine, ornithine, arginine and methionine. The end products of this process are water-soluble toxins that can be released via urine, sweat, and stool.
It is essential that the liver has all of these nutrients, as well as enough energy-producing fats and carbs, to fulfill its tasks on an ongoing basis. Otherwise, toxins accumulate in the body affecting a range of body systems which can lead to increased inflammation. Remember that vagus is essential for ensuring inflammation does not become chronic and have deleterious effects.
A strongly dysfunctional liver will often lead to fatty liver, which is becoming a much more common diagnosis, as well as an enlarged liver (hepatomegaly) and even potentially cirrhosis of the liver. The liver is the fastest regenerating organ in the body and when given the correct nutrients, it can recover quite quickly and begin functioning optimally to perform its many tasks.
CHRONIC STRESS
The autonomic nervous system (ANS), or involuntary nervous system, controls basic internal bodily processes automatically, such as digesting food, pumping blood, maintaining blood pressure, breathing, immunity and much more, including surviving danger.
The Parasympathetic branch of the ANS governs the long-term maintenance functions that allow you to live and be healthy, such as, digestion, hormone production, and strong immunity. The Sympathetic branch of the ANS is solely devoted to an instantaneous internal preparation to run or fight (fight or flight) in order to survive danger. such as running from a tiger or fighting to protect your family from a violent attacker.
The “fight or flight” stress system has helped humans survive on earth for tens of thousands of years. By activating this powerful mindbody system we have run from danger, or, fought to protect ourselves, since the beginning of human life on earth. But in modern life, this same stress system is killing us through stress related diseases such as heart attack, cancer, high blood pressure and diabetes. How do you explain this paradox?
For 95% of life on earth our dangers have been real and physical. The innate stress physiology prepared our ancestors to run from wild animals or attack them in the hunt. It helped them defend against invaders who wanted to steal the village food supply. Our stress system is well designed to protect us against dangers by running or fighting.
In modern times, however, the dangers are no longer physical. We no longer run from our fears because they arise in our minds daily in the form of worry and anxiety. We no longer fight our enemies, because the enemy has moved inside us in the form or anger, frustration, resentment and depression. “Fight or flight” has become “fear or anger” and this powerful system is responding to imaginary dangers for which there is no appropriate action.
Chronic Stress – Cortisol
Cortisol, the hormone of chronic stress, is more likely to be activated by your “everyday dangers”, and it is more involved in making you sick than adrenaline. Consider the well documented effects of chronic cortisol elevations on your mind and body:
- Increased appetite and food cravings
- Cortisol stimulates fat storage mainly around the abdomen
- Increased body fat – obesity
- Decreased muscle mass
- Insulin resistance and eventually diabetes
- Heart disease
- Increased blood pressure – high blood pressure
- Decreased bone density – osteoporosis
- Reduced synthesis of neurotransmitters
- Increased anxiety
- Increased depression
- Reduced concentration
- Mood swings (anger and irritability)
- Reduced levels of estrogen and testosterone – decreased sex drive
- Impaired immune response – frequent colds, flus, infections and cancer
- Memory and learning impairment
- Physical atrophy of brain cells – Alzheimer’s disease
- Increased symptoms of PMS
- Increased menopausal side effects
DYSFUNCTIONAL SLEEP AND CIRCADIAN RHYTHM
How well do you sleep? Do you wake up feeling rested and full of energy in the morning? When we sleep, we go through five cyclical stages of brain activity. Stages one and two are lighter sleep, often associated with the first 7 to 15 minutes of falling asleep. Stages three and four are the deep restorative sleep stages that are associated with muscle and tissue repair, growth and development, boosted immune function, and production of energy for the next day—essentially, all of the tasks mediated by the vagus nerve to help our bodies perform at their best the next day. Vagus nerve activity (measured through heart rate variability) has been shown to be significantly higher during stages three and four of sleep.
The fifth stage is rapid-eye movement (REM) sleep. During this phase, heart rate variability decreases. It has been shown that parasympathetic activity significantly decreases during this phase of sleep. Sympathetic activity predominates REM sleep, which is associated with formation of memories as well as dreaming.
Deep restorative sleep is the gym for the vagus nerve.
The vagus nerve trains during deep restorative sleep, stages three and four of the sleep cycle. Just as a weightlifter will train a specific group of muscles or a yogi will train their body to perform postures, the VN must train to function at its best. This means that if you are not getting a good, restful sleep at night, you likely are not entering the deep restorative stages required for vagus training—thus, you are not training the vagus nerve. As with most other nerves, if you don’t use it, you lose it. However, I prefer a different quote regarding nerves: If you don’t train it, you drain it (of the ability to perform optimally). Training your nerves is highly important to their function, and just as getting to the gym is important in training the nerves that activate your muscles, deep restorative sleep is a gym for the vagus nerve.
Mankind has been going to sleep when the sun goes down for millennia. Consequently, we all have deeply ingrained Circadian rhythms wired into our brains and bodies which influence energy levels, hormone production, neurotransmitter activity, memory, digestion, body temperature and more. When you go to sleep hours after sunset, you are disrupting these ancient cycles.
Getting to bed at an optimal time is essential for allowing the vagus nerve to train. Guidelines tell us that optimally, we need eight hours of sleep each night.
The vagus nerve acts as a peripheral clock based on the amount of food present in the stomach. There are certain times when sensitivity to stomach expansion is high and certain times when sensitivity is low. If you are going to sleep at a late hour, eating meals late at night, and feeling drowsy or lacking energy early the next morning, your vagus nerve is likely firing at inopportune times, leading to dysfunctional nerve firing.
You should eat at least 2 hours prior to bedtime so the stomach is empty.
LACK OF SOCIAL INTERACTION
We need to be around people. Face-to-face social interaction is supremely important for our health. If you’ve ever spent a few days at home, alone, I’m sure you started to feel a little down and moody. The vagus nerve is activated when you are in a social situation and interacting with people face-to-face.
My mentor, Sachin Patel, pointed out to me that in prison, the punishment for doing something wrong is to be put in solitary confinement—literally being placed in a small box by yourself, with no interaction for hours andeven days on end. We would rather be surrounded by other convicted criminals including murderers than be in a cell, all alone.
A 2009 study by Schwerdtfeger et al. in Health Psychology showed that heart rate variability—a great way to measure vagal tone—decreases in those with less social interaction and a depressed mood. Depression is associated with a lack of vagal tone. When patients with these same symptoms were put into social situations, their mood, heart rate variability, and autonomic control of the heart increased— namely, vagus nerve activity.
This finding was reinforced by a study in Biological Psychology, by Kok et al., just one year later. Adults recruited from a university had their vagal tone measured at the beginning of the program and again nine weeks later. Individuals with higher vagal tone scores predictably had greater increases in feelings of connectedness and positive emotions. Even more importantly, these individuals saw an increase in vagal tone at the end of the study.
Depression is directly linked to low vagal tone.
These studies show that our feelings of happiness and positivity are directly connected to vagus nerve activity and vagal tone. Those with higher vagal nerve activity actually feel more positive and experience social interaction in a more positive light. Depression and low mood are directly correlated to lower levels of vagus nerve activity.
This means that the more positive, in-person social interactions you have, the more you train your vagus nerve to function optimally. People who live in isolated environments with limited social interaction are not able to train their vagus nerves to their greatest ability and are more likely to suffer from health conditions caused by inflammation levels that cannot be controlled by the VN. Positive emotions build physical health while negative emotions lead to physical dysfunction and disease.
PART 4: MEASURING VAGUS NERVE FUNCTION
FOUR methods to measure vagus nerve function.
- heart rate variability,
- heart rate,
- breath pattern, and
- bowel transit time.
Heart Rate Variability
Heart rate variability (HRV) is the gold standard for measuring vagus nerve function. No single test is considered a stronger and more accurate representation of the activity levels of the vagus nerve and vagal tone.
Heart rate variability is the measurement of time, in milliseconds, between successive pumps of the heart—the time from the end of one heartbeat to the beginning of the next”. The amount of time between beats is heart rate variability and it is an important indicator of both cardiovascular and autonomic health. The more active your vagus nerve, the lower your heart rate will be, within an optimal zone, and the more variable the time will be between pumps of your heart.
Sympathetic innervation could elevate the heart rate to 120 bpm which will produce a lower HRV.
Parasympathetic innervation, on the other hand, lowers the heart rate and increases heart rate variability. Once the heart rate drops down to its normal resting state, HRV can be measured to determine just how healthy a person truly is and how well their vagus nerve is firing. Optimal heart rate is between 50 and 70 bpm, and HRV should be significantly varied between each pump.
The higher your heart rate variability, the more likely you are to have a higher level of fitness, cardiovascular health, and vagal tone. High HRV is also one of the best predictors of longevity.
PLEASE CALL MINDBODY MEDICINE CENTER TO MAKE AN APPOINTMENT FOR HRV TESTING – 480.607.7999
Resting heart rate and heart rate recovery
Resting heart rate is a simple measurement that tells you how well your body is functioning. If we consider that average resting heart rate is generally between 60 and 100 bpm. The lower your heart rate within the optimal range, the stronger the parasympathetic signaling to the heart.
Optimal heart rate in a healthy individual should be in the region of 50 to 70 bpm. Many athletic individuals tend to find their heart rate on the lower end, 50 to 60 bpm, while less active but still healthy individuals will tend to have a heart rate of 60 to 70 bpm. New research shows that a resting heart rate above 76 bpm is linked to an increased risk of heart attack. In fact, the risk of dying from any cause is correlated to an increase in heart rate in both men and women. Essentially, as resting heart rate goes up, the higher the chance of dying from any cause, especially one that is cardiovascular.
After exercise, it is important to measure how quickly your heart rate recovers to its resting rate. High-intensity exercise and training is known to lower resting heart rate over time, and consistent training is linked to faster recovery times. If it takes you a long time to recover following an exercise session, this is a sign of poor cardiovascular health and poor vagal tone; remember, vagus signaling is necessary to slow heart rate and maintain resting heart rate. Optimal recovery from exercise involves a drop of 12 bpm each minute, while unhealthy individuals take longer and tend to have a decrease of less than 12 bpm.
To measure heart rate recovery, check your resting heart rate a few times while relaxed. You can use a smartphone or wearable technology to get a relatively accurate finding and record this number. Then, perform your normal exercise or training routine and immediately test your heart rate at the end of the session, using the same method as earlier. Test again after 2 minutes, 4 minutes, and 6 minutes:
- after 2 minutes, your heart rate should drop by more than 24 bpm,
- after 4 minutes by more than 48 bpm, and
- after 6 minutes, it should be very close to your original resting heart rate.
This is, of course, dependent on how rigorous your training was and if it was aerobic (e.g., running) or anaerobic (e.g., weight lifting).
If you are tracking your heart rate and HRV regularly, you will notice an increase in HRV following exercise; your vagus nerve is highly active during the recovery process as it works to repair tissues. If aerobic andanaerobic training exercises and tones the muscles, heart, and spinal nerves, then recovery is the training session for the vagus nerve. The more you train, the more you recover, and the more effectively your vagus nerve will fire the next time you exercise. This is why recovery rates improve for those who exercise regularly: The VN is training to perform its job with greater effectiveness and tone.
Paradoxical Breathing Pattern Test
Are you using your diaphragm to initiate your breath? Have your breathing patterns become irregular and caused your vagus nerve to function less than optimally? This is a very simple test and a tool that you can use to train yourself to breathe with your diaphragm.
Sit straight up in a chair or lie down with your back on the floor. Place your right hand on the center of your chest and place your left hand on the center of your belly. Now take a deep breath in. If your right hand is moving more than your left hand, then you are breathing incorrectly. During the inhalation phase, our bellies should be rising and falling more than our chest is, so if we are breathing correctly, our left hand should be rising and falling more than our right hand.
Many people will find that their chest is moving more than their belly. This is a sign of paradoxical breathing and shows that someone is likely not using their diaphragm to breathe fully, deeply and correctly. If you arebreathing paradoxically, don’t worry, because you can train yourself to become an effective breather once again. It will simply take some effort and a daily practice to re-learn patterns that you had long ago when you were a child. See page 78 for breathing exercises.
Sesame Seed Bowel Transit Time Test
The sesame seed bowel transit time test can give us some information about how our digestive tract is functioning and if we need to make some changes to our health. All you will need for this test are one tablespoon of golden or yellow sesame seeds, one cup of water, a watch or clock, and a notepad and a pen. We know that our gut lacks the enzymes to digest and break down sesame seeds (similar to corn), which is what makes them so effective for this test. We also know that the vagus nerve is the driving force for peristalsis and keeps the digestive tract moving at an optimal pace. Any variations from this pace can signal a loss of VN control or some other digestive dysfunction.
Here’s how to do the test.
- First, add the sesame seeds to the cup of water and stir it around.
- Next, drink the cup of water with sesame seeds in it, being sure to not chew the seeds.
- Write down time and mark it in your notepad or in your phone.
- Wait until the next time you need to go to the bathroom for a bowel movement.
- Each time you have a bowel movement, look for sesame seeds in your stools.
- Mark down the times and continue checking until you no longer see any seeds.
The optimal time in which to see the seeds begin appearing is around 12 hours after ingestion and the latest is around 20 hours after. Seeing seeds 16 hours after ingestion indicates optimal digestive sequence and function.
If your body is pushing the seeds out very quickly, your digestive tract is not working hard enough and the VN is likely not firing optimally. If your body is very slow to eliminate the seeds, then vagus activity is certainly decreased. In either case, testing of the gut microbiome is highly recommended, as it can uncover the cause of poor bowel transit time and potentially poor vagus nerve signaling.
PART 4: EXERCISES TO ACTIVATE VAGAL FUNCTION
Breathing Exercises
The first and most effective way to positively affect your vagus nerve is to learn to breathe correctly. Simply put, rapid, shallow, chest breathing is a sign of stress, which activates the sympathetic branch, while slow, deep, belly breathing is a sign of rest, which activates the vagus nerve.
Breath is our one window into the autonomics.
—Dr. Jared Seigler
Most people in modern stressful society do not breathe correctly. Researchers estimate that 75 – 80% of people unconsciously overbreathe. If you haven’t yet completed the paradoxical breathing pattern test on page 76, I highly recommend doing it now. Correct breathing patterns are directly linked to autonomic nervous system function and altered breathing patterns tell the body that it is under stress. This fact is even more amplified once you realize that the average person takes approximately 23,040 breaths per day.
Multiple research studies have shown that slow breathing exercises are highly effective in improving heart rate variability. One study showed that slowing your breath rate to six full breaths per minute for five minutes was effective in increasing HRV immediately. If this is individualized, the effect on HRV is even more effective. Determining the slow breath rate that is optimal and feels right for you individually will have the greatest positive effect on your HRV levels.
Here are simple steps to practice this exercise:
- Sit up straight without allowing your back to rest against anything.
- Exhale completely to remove all air from your lungs.
- Put your right hand on your chest and your left hand on your belly, just above your belly button.
- Take a deep breath in through your nose for five to seven seconds, allowing only your belly to rise (feeling only your left hand rising).
- Hold that breath for two to three seconds.
- Exhale through your mouth for six to eight seconds, allowing your belly to fall (feeling only your left hand falling).
- Hold your breath, without any air entering your lungs, for two to three seconds.
- Repeat steps 4 through 7 as many times as you feel comfortable or for a set period of time.
Take five minutes per day to practice deep belly breathing on your own and your body will thank you. For best results, perform this practice multiple times per day, especially during periods of stress. Even a single minute of concentrated focus on slow, deep breathing can have significant positive effects on your mood, stress levels, and overall health. Work to focus your attention on breathing in through your nose rather than your mouth to make this exercise even more effective when you are practicing it.
Breathing Patterns During Sleep
The average person requires between seven to eight hours of restful sleep per night, during which they take approximately 7,200 breaths. This is important, as nearly one-third of our breaths are taken while we are not awake. We can train ourselves to breathe optimally when we are conscious and in control of our actions, but what about when we are asleep?
Snoring is very common; about 25% of women and 45% of men have habitual snoring. It occurs because the tongue is to big for the mouth. This appears on a medical examination as scalloping or indentations on the lateral edges of the tongue due to the tongue pressing up against the teeth. During sleep the tongue relaxes and partially obstructs the flow of air into the lungs which produces the snoring sound. If the obstruction becomes complete there is no oxygen delivery to the body and we awaken in a startle, which is called “sleep apnea”. Medical sleep studies document the phases of sleep and the degree and frequency of sleep apnea.
Twenty-six percent of people between the ages of 30 and 70 suffer from sleep apnea. ‘Witnessed breathing pauses during sleep’ and ‘excessive daytime sleepiness’ are the most common symptoms. If you have chronic snoring that is loud enough to wake a bed partner, talk to your doctor. Obstructive Sleep Apnea (OSA) is a medical diagnosis based on a sleep test score, and its usual treatment is a CPAP (continuous positive airway pressure) mask. Apnea means absence of breathing for 10 seconds or longer, and the obstruction is rooted in the choked airway inside a structurally impaired mouth.
Fifty percent of high blood pressure, 30% of heart attacks, 60% of strokes, and 25 % of heart failures have obstructive sleep apnea as an underlying problem, reported a 2003 study in the Journal of American College of Cardiology. In 2006, the American Academy of Sleep Medicine stated that “Oral Appliances are a simpler alternative to CPAP… with robust studies demonstrating their efficacy.”
Improving your sleep
A restful night of sleep has been shown to improve autonomic balance through heart rate variability studies.
Eliminate Blue Light Exposure in the Evenings
Light wavelengths change throughout the day, and our bodies have adapted to their signals. When the sun rises in the morning, light is quite warm, in the red/yellow wavelengths. By noon, the light is much more blue and sharp. Once again, in the evenings, when the sun is setting, the light turns toward a red/yellow hue. These are the signals that our body uses to tell us the current time of day, as well as which hormones and signals to secrete at precise times.
Our screens, including the laptop, TV, phone, and tablet, all emit a blue wavelength of light. If we look at our screens each evening right before bed, we send a signal to our bodies that the time is actually noon. This will slow the release of melatonin, an important hormone required to help us relax and fall asleep soundly. Some devices now come with built-in blue-light filters, but most do not.
To reduce blue light exposure while still using devices and screens during the evenings, you can:
- Enable Night Shift on your Apple devices
- Download the Twilight app on Android devices
- Download f.lux or Iris on your computer (Mac or Windows)
- Use blue-blocking sunglasses if you are watching the television
For blue-blocking glasses, I recommend using the TrueDark Twilight sunglasses, which are the gold standard of blue-light blocking technology. Instead of looking at your screen at night, I recommend reading a physical book or spending device-free time with loved ones or friends, as social connectedness is another great way to improve vagus nerve function.
Shut Off Electronics at Night
One of the best things I have ever done for my health was to cancel my cable TV subscription. It forced me to stop watching TV at night. I have since taken steps to reduce electronic use in the evenings and nights, and get noticeably better sleep having done so.
Charging your devices such as cell phone or tablet in a different room, shutting off Wi-Fi routers with an automatic timer, and even putting your devices on flight mode are great ways to stop using them in the evening. Also do not sleep with your cell phone on the bedside table.
Don’t Eat or Drink Too Late
Nighttime bathroom breaks commonly break up restful sleep. If you eat or drink later in the evening, then you are preparing your body to need to use the washroom at night. Instead, have your final meal at least two hours before you sleep and your last drink of water at least one hour before bedtime. Your waistline and your energy levels will thank you the next day!
Love Your Space
Sleeping in a clean, organized space is imperative to improving your sleep quality and your health. When your bedroom is a mess, you can’t help but go to sleep thinking about the cleaning and organizing that needs to be done. This negative energy creeps into your mind and makes your sleep restless, which is simply added stress on the body and an easy way to turn off the parasympathetic recovery system at night.
Have a feng shui assessment done on your space to ensure it is organized in an energy-positive way to help you feel great and allow you to grow. Ensure that you clean and organize your space regularly, as this has a direct effect on your mood and energy levels. I recommend reading The Life-Changing Magic of Tidying Up by Marie Kondo to learn more about how a clean space transforms the energy in your body.
Sleeping on Your Side
A 2008 study by Yang et al. published in Circulation Journal compared the HRV levels of different sleep positions. The study was done to determine the best position for patients dealing with coronary artery disease compared to those without any blockages in their coronary arteries. The researchers found lying on your back is the worst position for HRV levels, both for test and control patients, while lying on either side showed significant improvement in HRV levels. Most interestingly, sleeping on the right side was found to be the best for vagal modulation, especially in the control group.
What this essentially means is that sleeping on your back or lying on your back for a longer period of time, will have negative effects on vagus nerve function, while lying on either side (right side preferred) will actually allow you to increase vagus nerve tone. This is because when you are lying on your back, your airway is more likely to close, as your tongue can fall backward due to the pull of gravity. This is not nearly as easy when you are lying on your side. Remember, an open airway is essential for control of breathing, both in terms of breath rate and depth of breath. To make it easier to sleep on your side, I recommend placing a pillow between your knees while you sleep. This will force you to stay on your side while you are asleep and will not allow you to shift to sleeping on your back.
Cold Exposure
Have you ever jumped into a lake or pool, only to realize that the water is frigid and freezing you to your core? Your teeth begin chattering and your body begins to shiver uncontrollably. Your breath is completely out of your control as well. You take extremely shallow breaths and are unable to rest your diaphragm enough to calm down and breathe deeply.
As you can imagine, this scenario is great for activating your sympathetic nervous system and the fight-or-flight response. Your body is fighting to survive in the short term, and this has an immediate effect on how your body reacts. Your breath becomes shallow and rapid, your heart rate increases, and your body does not desire to digest optimally during this time. All this short-term effort is meant for survival.
What you may be surprised to hear is that this has the amazing effect of activating the parasympathetic nervous system in the long-term. Continuous acute exposure to cold, or cryotherapy, teaches you to regulate your breath, which has an overall positive effect on vagus activation and significant anti-inflammatory effects throughout the body.
Periodic cold exposure is one of the best and easiest ways to activate and heal a lost vagus nerve. The simplest way to incorporate this into your life is to add cold exposure to your showers. One great tip I give to many of my patients is to take a normal shower, then at the end of the shower, turn the temperature down to as cold as possible and let it hit you on your head and the back of your neck for the final minute of your shower. It will initially be shocking to your system and will change the way you breathe. Your goal during this time is to work on controlling your breath and taking as many deep belly breaths as possible. If you can train your body to breathe through the cold, your vagus nerve will become very strong, and your body will have an optimally functioning parasympathetic nervous system and vagus nerve. As this minute becomes easier, you can add one or two minutes per week of cold exposure until your entire shower is spent in ice-cold water and there is a huge smile on your face!
Cryotherapy is an emerging and proven science that is used to help reduce inflammation and activate healing via the parasympathetic nervous system. Most professional athletes, as well as performers such as Tony Robbins, use cryotherapy following each game or performance. Mr. Robbins swears by it for his own health and has found it to have significant healing benefits.
Even Wim Hof, the creator of the Wim Hof method, incorporates cold exposure into this method for its amazing healing benefits. He is known as the Iceman, as he regularly engages in ice baths with his clients and teaches about the benefits of cold exposure. If you feel that cold showers have become redundant and too easy, try going out for a hike on a mountainside in just a pair of shorts and boots. A Google image search for Wim will show him doing just that.
Humming or Chanting
Another way to activate your vagus nerve is to stimulate and use the voluntary muscles that it signals. By activating these muscles, you stimulate the brainstem centers that send signals through the vagus—not just the muscle control centers, but all the others around it as well. Humming and chanting activates the laryngeal muscles, which get signals directly from the superior and recurrent laryngeal branches of the vagus nerve. They allow our vocal cords to tighten and loosen based on muscle tension, thus giving us a level of pitch in our voices. When we practice humming deep in our throat, we are activating and vibrating these muscles and stimulating vagus to send these signals.
Perhaps you are aware of the sacred Hindu syllable “OM” that is used to create a deep vibration in the throat when recited out loud. The vibration of “OM,” which is said to vibrate at the resonance level of God, has a strong spiritual affiliation in the practice of Hinduism. In other cultures, simple words are used such as Amin, Ameen, and Amen; however, they seem to all mean the word of God.
Chanting OM stimulates the laryngeal muscles of the throat and vocal cords, allowing stimulation of the motor fibers of the vagus. If done for long enough and with enough strength, it can be a strong method of stimulating the other signaling components of the nerve. It allows us to control our breath, slow down our thoughts, and center ourselves to the point of extremely deep relaxation, and has been shown to improve digestion and inflammation levels in the body. Humming or chanting the word “Om” prior to a meal can be a great way to calm yourself down, align with the universe, and stimulate vagus nerve activity to the digestive tract and other visceral organs. Practicing “OM” during other times, including following a stressful event, is a valuable tool in decreasing stress levels and sympathetic activation following this stressful event.
There are other words to hum or chant that can actively stimulate these muscles and improve vagus nerve signaling, but “OM” is one that I have personally found to be highly effective, as the vibration of the throat muscles is highly evident during the practice.
Activating Gag Reflex
Along the same lines as humming and chanting, activation of the gag reflex is another way to stimulate the muscles innervated by the vagus. Also known as the pharyngeal reflex, this reflex, which involves a loop of nerve activation to work optimally, is required to protect us from choking.
When an object that we are not aware of enters our mouth and touches our soft palate (the soft part at the back of the roof of your mouth), a very fast sensory signal is sent through the ninth cranial nerve, up to the brainstem, and to the motor aspect of three different cranial nerves. The first of these nerves is the pharyngeal branch of the vagus, which immediately contracts the three pharyngeal muscles at the back of the throat to stop the object from entering the body farther and potentially getting stuck in the airway. Cranial nerve five and cranial nerve twelve are also stimulated and cause the jaw to open and the tongue to thrust forward to push the object out.
Voluntarily activating the gag reflex will send an immediate signal to the vagus and the other nerves to keep them signaling quickly and optimally.
The best time to do this is twice per day, while you are brushing your teeth. You can use the toothbrush to touch the soft palate and stimulate this reflex. This is a great and simple option that is known to have a direct effect on the signaling of VN. As we have a set of cranial nerves on either side of our body, stimulating the soft palate on both sides is necessary to receive the full benefit of this exercise.
Gargling
When I was a child, my father often encouraged me to gargle with saltwater after brushing my teeth in the morning and evening, just as he has practiced every day for his entire life. He used to tell me that it was good for my health—yet I would laugh it off and make light of this advice. Interestingly, he was on to something. I should have known; he is a very healthy septuagenarian.
Gargling is the act of holding a sip of water in the back of your throat and swishing it around with vigor. It requires activation of the three pharyngeal muscles at the back of the throat, and as such, it is another method of stimulating the vagus nerve through muscle activation. As my father would consistently remind me, practicing this twice per day after brushing teeth is a great way to easily harness this tool.
For best results, gargling with extra vigor, to the point where your eyes begin to form tears, is optimal. When your vagus is firing, it actively sends signals from its brainstem nuclei that activate some adjacent nuclei as they get stronger. In this case, the superior salivary nucleus is being stimulated, which triggers the glands around your eyes to produce fluid that becomes tears. If you are gargling hard enough to make yourself tear, you are doing this correctly and having a great effect on your vagus nerve.
Adding some salt, such as Himalayan pink salt, to the water you are using to gargle is also a great option. Gargling salt water has been shown to have antibacterial effects and can help eliminate some unwanted bacteria from the mouth and upper respiratory tract. Using essential oils, such as oil of oregano, in your water is another great option with very similar effects.
Yoga or Pilates
Yoga and Pilates are not meant to just exercise the body, but to calm the mind and regulate the breath. These methods exercise optimal voluntary breath regulation while increasing external stressors and teaching you how to control your breath.
Most yoga sessions are bookended with a slow deep belly breathing exercise. The idea is to teach you to maintain your breath pattern while your body is held in different positions. Each of these positions engages the body with a different type of physical stressor. To increase the level of stress within this practice, we have learned to use heat and humidity, which are even more engaging. Moksha and Bikram yoga are two examples of this.
If we can learn to maintain a slow, deep belly breath during times of stress, our bodies are able to function at much greater levels. If we train ourselves to handle voluntary stressors by maintaining our breath, then we can be trained to maintain composure and handle other stressors with significant ease.
Pilates was created as a practice around learning to breathe correctly. If we are breathing paradoxically during periods of low stress, our bodies will not be able to handle periods of high stress. Both yoga and Pilates, when taught with a focus on the breath, are great tools for optimizing breathing patterns, improving inflammatory responses, and activating the VN to function optimally.
Mindfulness Practice
Prior to starting a task, do you take a moment to sit still, close your eyes, and focus your attention? Do you ensure that you are putting 100 percent of yourself into the task at hand? When you are resting, do you take a moment to become grateful for your surroundings?
Mindfulness is exactly this: taking the time and making the effort to pay attention to what you are doing and what is happening around you. Many of us jump from task to task, or put out one fire after another without paying attention to what is going on around us. We get so caught up in our own minds that paying attention to a single task and giving it our full attention gets put on the backburner; it feels like a waste of time and effort to do this.
Many health care professionals, myself included, are guilty of this. We go from patient to patient or appointment to appointment, forgetting or not giving our full attention to the fact that someone is trusting us with decisions involving their health and their life. Becoming a functional medicine doctor has allowed me the opportunity to affect the lives of my patients in a positive and deep way, and as such, I am far more conscious of the attention I can give each of my patients. Prior to bringing in my next patient, I take a couple of minutes to review my notes, remove any distractions from my vicinity, and clear up tasks involving other things.
Once I do that, I take a moment to remember that each patient trusts me to help them achieve their goals in health and in life.
Mindfulness practice means performing each task to your greatest capability with 100 percent of your attention directed at that task. It means taking in your surroundings, being aware of everything that has brought you into that exact moment, and being grateful for it. The ability to practice mindfulness cannot occur when we are stressed out, inflamed, and in pain. Our sympathetic nervous system tends to hijack our attention and prevent us from focusing on what we are doing. If you actively practice mindfulness throughout the day, you are focusing on your breath and how you can achieve each task at hand. This shifts the balance toward the parasympathetic nervous system and allows the VN to do its job.
Approaching a task mindfully means doing one thing at a time with full attention and finishing it before moving on to the next task. Eating mindfully allows you to feel satiated and not overeat. Mindful relaxation allows you to feel rested and rejuvenated sooner than you’d imagine. All of these require the vagus nerve to be active and engaged, as we must be able to rely on so our bodies can rest, digest, and recover. Multi-tasking is exactly the opposite of mindfulness.
Becoming mindful of what I am doing, eating, and feeling as each task approaches has been the most positive change I have made in my life, and it is by far the number one reason my health outlook became more positive. It has been a major needle-mover for me and for countless others around me, and I’m certain that it can make profound positive changes in your life as well.
Meditation
Meditation is similar mindfulness. It is the art of paying attention to your breath and teaching your attention to not follow each thought that pops into your mind. Our brains are designed to think and form dynamic, ingenious connections between our thoughts and actions. Meditation teaches us to listen to our hearts and focus on our breath, learning to become observers of our thoughts rather than victims of their fluidity.
Rather than debate the countless methods of meditation, I want to discuss its benefits. Heart rate variability studies have shown that meditation has significant positive benefits on vagus nerve function because as we meditate, our attention moves toward our breath. There are many different types of meditation but those that are focused on the breath are typically best for improving HRV levels. These include breathing meditation, lovingkindness meditation, vipassana, and mindfulness meditation.
One interesting tidbit of information I found through my research is that HRV only showed improvement in patients who did not label themselves as perfectionists. In the International Journal of Psychophysiology, a study by Azam et al. found that control patients were far more likely to have positive changes in HRV levels compared with those who self-identified as perfectionists. Essentially, “perfectionists” were so focused on meditating perfectly or in the correct way that they didn’t allow themselves to relax and benefit from the practice itself. One of the most common things I hear when I ask my patients about meditation is that they are “not able to do it correctly.” This perfectionist attitude is exactly what is stopping them from realizing the benefits. When practicing meditation without any expectations or preconceived notions about “the correct way” to do it, it is easier to benefit from the practice.
For beginners, I recommend using guided audio meditations found on YouTube or through an app on your phone. I recommend Headspace, Oprah Winfrey and Deepak Chopra’s 21-day meditation experience, Calm, and Insight Timer. For those who want feedback on the meditation practice, HeartMath’s Inner Balance is a great tool to help you determine if you entered a state of congruence, which is measured through heart rate variability. Another tool for those interested in getting direct information is Muse, the meditation headband, which measures brainwave activity and gives you real-time audio feedback. These are add-on tools and are not at all necessary to practice, but they can be a good investment for those who typically strive toward perfection.
READ MORE ON THE MANY BENEFITS OF MEDATION TO BODY AND MIND
https://healmindbody.com/knowledges/meditation-prescription-for-health-and-well-being/
Laughter and Social Connectedness
If you knew that laughing more would improve your health, would you do it more often? Remember the last time you had a good laughing session with friends. Did you feel great for the next few hours? Did you sleep better that night? Did you wake up feeling great the next morning?
Ongoing research repeatedly shows laughter and laughter yoga to be very effective in improving mood and heart rate variability. We tend to use our diaphragms when we laugh with vigor and enjoyment, and in turn, we exercise our ability to control our breath rate and ensure we can normalize our breathing patterns. This is exercise for the vagus nerve.
Making vigorous laughter a regular occurrence is a great and very enjoyable way of improving vagus nerve function. I make a point of watching funny videos or going to comedy shows as often as possible to feel connected socially, and to enjoy the health benefits of laughter. Taking laughing yoga classes in your community, meeting with friends regularly to exchange fun stories, and turning on a comedy movie are all great options to laugh more. Social connectedness is directly involved with this, as we are more likely to laugh out loud when we are in the presence of others, especially friends and family. Social connectedness is one of the greatest determinants of health and can be even more important than the food you eat.
People want to be around other people. When we feel lonely and disconnected from others, our mood and health are both negatively affected. We tend to enjoy the company of others and prefer having conversations with real people, face-to-face. When we are around others, we tend to laugh more, smile more, and feel more relaxed.
We feel even better when we spend time with people we resonate and share values with. I was recently able to take my family to a Living Proof Team Retreat in Minnesota, which was an amazing experience. The beautiful natural environment and surroundings were coupled with spending time with team members that share the same values that I do. We were taken care of by the team at Point Retreats, another spectacular group of individuals that values bringing people back to healthier and happier lives. At the end of the trip, we were all very happy and relaxed, regardless of the stress of travel.
If you are feeling lonely, down, or simply disconnected, find a way to spend time with others and connect to people with similar values to yourself. If physical fitness is an important value, join a gym or attend a yoga class with friends. If communication is an important value to you, then join a toastmaster’s group and practice your public speaking skills with supportive, like-minded individuals. If you value quality time with others, then go to a movie or a meal with friends so you can converse and have a great time. There are 7 billion people on the planet and countless activities and interactions that allow you to connect to these people.
It is believed that as we age, we laugh less, but the healthiest people I know make a point of laughing more. And in the blue zones, the regions around the world with the highest rates of longevity (with many people living past 100 while still being physically active), social connectedness is a common theme.
So get out, enjoy social experiences with those around you, meet new people, exchange fun stories, and laugh as loud and as often as you can. Doctor’s orders!
Listening to Music
Don’t you feel good after listening to some great music and singing along? This is because your body is actually feeling relaxed and is able to perform recovery processes during and after this time. It’s the same reason why we love to belt out the lyrics to our favorite tunes while sitting in our cars or stuck in traffic.
A 2010 study by Chuang et al. showed that cancer patients who participated in a 2-hour music therapy session that included singing, listening, learning, and performing music showed significant increases in heart rate variability measures, and thus in vagus nerve and parasympathetic nerve activity. Another study by Lin et al. in 2014 used HRV to show that Mozart’s music can improve parasympathetic nerve function. Much of this research has been completed with children diagnosed with epilepsy, a common seizure disorder. Listening to Mozart’s music, especially Mozart’s “K.448” sonata for two pianos, showed a decrease in seizure recurrence and brain changes.
Next time you are sitting in traffic and feeling stressed that you are late for a meeting or for work, turn on some good music and let your body move and sing along with it. You will inevitably feel more relaxed and lessstressed, and you will still get to your meeting at the same time. If you are at home and feeling out of it, play Mozart in the background and notice how you feel after.
Music has healing power. It has the ability to take people out of themselves for a few hours.
—Elton John
Smart Dietary Choices
As the research is slowly becoming clearer, we are discovering that there are foods that can have a negative impact on our cellular and digestive health and which have a higher likelihood of increasing inflammation levels. Most of these are highly processed foods; foods that are contaminated with antibiotics, hormones, herbicides, and pesticides; and foods that are genetically modified. Avoiding these foods is critical in reducing the risk of damage to the gut lining, liver detoxification system, and health of each of our cells.
When choosing healthy and smart foods, I recommend organic, locally grown fruits and vegetables; lean, free-range chickens and eggs; lean, grassfed and grass-finished beef; non-GMO grains like brown rice and quinoa; and organic nuts and seeds. For a majority of people, a green, clean, and lean diet made with healthy fats and minimally processed food is the best place to start. To learn more about dietary options, I recommend reading Food: What the Heck Should I Eat? by Dr. Mark Hyman. Follow his protocol for four weeks, then reintroduce one food at a time. Remember, your diet needs to be individualized to your needs and preferences. Vegan, autoimmune paleo, paleo, and ketogenic diets are all helpful, but a diet should be suited to what you need. Remember that green, clean, and lean are my personal three rules when shopping at the grocery store or farmer’s market.
When looking to specifically increase vagus nerve function, foods that contain nutrients helpful to the production of ACh are essential. Acetylcholine is the major neurotransmitter used by the vagus nerve, and low levels can contribute to suboptimal vagus nerve activity and signaling. Nutrients that are necessary to allow ACh production are high in choline, such as egg yolks; high-quality cooked organ meats like beef, chicken, and turkey livers; and soy lecithin, a common food additive.
Another effective tool to use in improving vagus nerve function is to give it a rest—literally, let your vagus nerve take some time off. Intermittent fasting and time-restricted eating are effective tools in improving heart rate variability. This is a tool I personally use to balance blood sugar, improve energy levels, and limit the amount of stress on my body. Intermittent fasting has been shown to increase HRV, a sign that vagus nerve function is optimized, and health is improving over the long term.
Daily Movement or Exercise
Our bodies are built to move. Muscles are some of the most important and most overlooked organs of the body, and muscle cells are the best at helping us balance our blood sugar and body fat levels—if we use them. The issue is that most us sit and lack movement for a very long time each day, and then we sit in the car, and sit on the couch, and repeat this lack of movement on a daily basis.
Practicing some level of movement, preferably one that helps increase your heart rate by increasing bodily stress levels for a short period of time, helps improve parasympathetic nerve activity. There are times when both the sympathetic and parasympathetic systems can be activated, and postexercise recovery is one of these circumstances. During the recovery state, we are optimizing our breathing pattern, which increases signaling to the muscles of the airway to increase patency, trains the heart to become stronger and pump out more blood with each pump, and allows us to shift back to a parasympathetic state on a regular basis.
Moving your muscles and getting your body to do things that stress it out on a daily basis will teach the body how to recover from the stress more quickly, while also helping you balance energy levels and macronutrient fuel sources. Use your muscles to make your body do things, preferably outdoors.
Sunlight Exposure
Exposure to sunlight throughout the day is directly linked to your sleep. Our bodies are genetically programmed to work based on the amount and type of sunlight that enters our eyes and skin. It has a direct effect on how we function on a cellular level. If we spend an entire day indoors under artificial lighting with limited exposure to true sunlight, we are depriving our cells of optimal signaling and function.
Light exposure during the day is directly linked to improved HRV levels. Our eyes and skin prefer to receive signals from red, infra-red, and yellow wavelengths during sunrise and sunset, while they prefer blue, green, violet, and ultraviolet light during the middle of the day. Sun exposure will do this naturally, while our workplaces, cars, and homes will not—at least not yet. Circadian lighting technology is being developed by many companies at the time of this writing.
As sunlight is directly linked to HRV levels, it is highly recommended that you go outside and get direct sunlight on your skin each day. Doing this at several different times of day is an even better option. The best times to get outside are within 30 minutes of sunrise, two or three times during the day, and within 30 minutes of sunset. Even better, spend the entire day outdoors whenever possible. You are far less likely to burn your skin during the day if your body senses the sunrise and is pre-conditioned to the UV light that we experience during the daytime.
Nutritional Supplementation
Because our diets lack nutrient density and our environments have decreased our microbiome diversity, supplementation is a smart way to ensure our cells get the correct micronutrients and signals that will allow them to function optimally. Contrary to prior belief, supplements are not a waste of money, as long as they are taken by the right person for the right reason. Using functional lab testing, we can determine the best supplements for each individual to reach their optimal cellular function. There are, however, some basic nutrients and signaling supplements that can help all of us. Note that this is intended as general advice. You should speak to your primary health care practitioner prior to starting or stopping any medications or supplementation that has been prescribed or recommended to you.
Probiotics
Antibiotic use, C-sections, and diets of poor nutrient density have led us to have poor bacterial diversity and low levels of good bacteria in our gut. Testing to confirm which bacterial species are present is the optimal choice, but the majority of us will need to support our gut and skin microbiome using probiotics. Probiotics are bacteria that are produced externally. When ingested, they can help improve bacterial diversity and growth of good bacterial colonies. These are different from prebiotics, which are generally derived from fiber and act as food for the bacteria to produce vitamins and minerals for us.
When choosing a probiotic, I recommend spore-based, naturally formed bacterial species, such as Bacillus, which are formed naturally in soil. These probiotics help to fill the voids that are left when other bacteria die off. Probiotics that must be refrigerated tend to have a very low absorption rate (5 to 10 percent) when compared with spore-based probiotics and those that don’t need to be refrigerated. The question that I ask of probiotics that must be refrigerated is that if the bacteria can’t withstand room temperature, how will they get past the acid of the stomach and live through our higher body temperature?
MegaSporeBiotic is my preferred probiotic option for most patients on a maintenance protocol. It has a very high absorption rate, does not need to be refrigerated, and contains Bacillus species that can help fill the voids left by many different types of missing bacterial species, not just Lactobacillus and Bifidobacteria, which are the main species covered by the majority of probiotics.
Omega-3 Fatty Acids
High-quality omega-3 fatty acids are commonly deficient in modern Americans. Often called fish oils, they are derived from fish, but can also come from certain plant sources, which are the preferred source for vegans.
When choosing a high-quality source of omega-3 fatty acids, I highly recommend going for the triglyceride type, as it is natural and contains a high quantity of EPA and DHA, both of which are necessary for brain function and anti-inflammatory effects in the body. EPA and DHA improve nerve function, including VN function, as they are required for myelination of nerves and provide anti-inflammatory effects. Supplementation with omega-3 fatty acids has also been shown recently to improve heart rate variability in obese children.
READ MORE ON FISH OILS
https://healmindbody.com/do-you-really-need-fish-oils/
Parent Omega is a supplement used at MindBody Medicine Center which contains the plant oils required for your own body to synthesize Omega 3 oils.
5-HTP for Serotonin
Anxiety and depression are very common in North America today, and research shows that anti-depressant medications may be causing more of a problem. A long-term study published in 2014 by O’Regan et al. showed that patients with depression had a reduced HRV, and that these rates are actually made worse by anti-depressant medications that are trying to improve serotonin levels.
The precursor to serotonin is called 5-HTP. It can be used as an effective supplement to allow your body the opportunity to build its own serotonin. Most cases of depression are due to serotonin imbalance, and organic acid functional testing, which I use with nearly every patient that comes into my office, can tell our patients whether they have too much serotonin and use it up very quickly, or if they are running low on its production.
One thing to keep in mind is that the majority of serotonin synthesis occurs in the gut microbiome. A balanced microbiome will produce a good amount of serotonin and allow mood to be balanced while an unbalanced microbiome will do the opposite, leading to a higher risk of mental health issues.
Coffee Enemas
In more severe cases of bowel motility issues, especially when people are chronically constipated and unable to void their bowels for quite some time, enemas can be highly effective. A strong coffee enema is a great and simple option with a very high efficacy level. Dr Datis Kharrazian writes in his book, Why Isn’t My Brain Working? , about how coffee enemas strongly stimulate the nicotinic acetylcholine receptors, the same receptors that the vagus affects through its release of acetylcholine. Caffeine stimulates these receptors in the gut, causing an artificial urge to void the bowels through a bowel movement.
To effectively use this tool to re-train vagus, you must suppress that urge for as long as possible. By suppressing the urge to go, you cause an axis in your brain to fire (frontopontine vagal enteric axis), thereby forcing the vagus and brain to become highly active and learn to reactivate these gut motility nerves. If you do this regularly over time, the vagus nerve will be retrained and will be able to release stools without needing the external support of a coffee enema.
If chronic constipation and poor liver detoxification are issues for you, then this process is an effective tool to help you clear out the bowels and get the toxins out of your body more efficiently. Doing this correctly and suppressing the urge to void for as long as possible, you will re-train the vagus to learn how to fire and affect the nerves that control gut motility.
PASSIVE METHODS TO ACTIVATE THE VAGUS NERVE
In addition to all the active exercises that you can perform on your own, there are passive treatments that can have profound effects on the activation of the vagus nerve. Some of these involve using certain equipment or visiting a health care provider, while others you can do in the comfort of your own home. Remember to discuss these options with your primary health care provider prior to beginning any type of treatment.
Auricular Acupuncture
Acupuncture is an effective form of therapy for many conditions, and I have seen its spectacular effects firsthand using it with my patients as a hands-on chiropractor. If you recall, one of the four types of signals that vagus controls is sensation to specific parts of the external ear, or auricle: the entire concha, the crus of the helix, and the tragus. As such, stimulation of these specific regions will have effects that can stimulate the function of the vagus nerve.
A significant and growing body of research shows that acupuncture and transcutaneous vagus nerve stimulation through the auricular branch of the VN yields positive effects in many patients suffering from depression, anxiety, epilepsy, LPS-induced inflammation, tinnitus, and highly active pain receptors. The best part about this form of treatment is that it is effective without being invasive.
There is also a growing trend in the health care community centered around the activation of the vagus nerve through electrical stimulation. This is done by surgically implanting an electrical stimulation device on the vagus nerve itself. Acupuncture is significantly safer than and just as effective as this invasive technique. In fact, auricular acupuncture and implanted vagus nerve stimulation devices engage the exact same neural pathways. Given the choice, I would personally choose acupuncture every time.
Massage Therapy and Reflexology
Massage therapy is a great tool to help us relax. Immediately following a good massage, I personally move slower, breathe deeper, and see the world in a more positive light. Unless your therapist is hitting some severely tender spots, most people feel quite relaxed and refreshed following a massage. This feeling can be the epitome of parasympathetic activation and sympathetic deactivation.
Not surprisingly, many different techniques of massage have been linked to increases in HRV levels or improved vagal tone including Chinese head massage; traditional Thai shoulder, neck, and head massage; traditional back massage; and even self-massage.
For my many patients that have trouble getting relaxed, I also recommend trying reflexology. Ever since my mom learned to practice reflexology, I had been open to the possibilities and was the first to volunteer as a patient when she was learning. Every time she would work on my feet, I would fall asleep, even as a teenager. For this reason, I was not surprised when I found a research article showing that patients treated with foot reflexology showed significantly increased HRV levels and lower blood pressure levels 30 and 60 minutes after treatment. Passive therapies like massage therapy and reflexology can have enormously beneficial effects on our health when they help us to relax and increase vagus nerve function.
Visceral Manipulation
Visceral manipulation (VM) is a less common therapy but one that is very effective when practiced correctly. Typically practiced by osteopaths, chiropractors, naturopaths, and other health care providers, VM is the gentle physical manipulation of the organs of the abdomen, thus increasing blood flow to areas that are not functioning optimally.
Visceral manipulation therapists use gently applied hands-on therapy to find areas of altered or decreased motion within the viscera and release restrictions within these visceral organs. The treatment involves a gentle compression, mobilization, or elongation of the soft tissues. Finding a certified visceral manipulation therapist in your area may be a good idea, especially for those people dealing with dysfunction with detoxification or with liver, gallbladder, or kidney pain.
Chiropractic Care
Neck and back pain are common around the world. They have become far more prevalent over the last 20 years as our jobs and careers have become significantly more sedentary and the majority of them require us to sit in front of a computer for hours on end. As a chiropractor, I have treated thousands of patients dealing with pain in their neck and back as a result of sitting in this position for many hours each day.
When joints are not moved through their full range for a long period of time, the muscles around them can become quite stiff and weak. As a result, the joints can become mildly misaligned and lead to pain. Mechanical joint pain caused by lack of motion is more common than pain from overuse of a joint. In my practice, I have found it to be true – If you don’t use it, you lose it—function of a joint, that is.
A 2015 study in the Journal of Chiropractic Medicine showed that in patients with neck pain, spinal manipulation performed by a chiropractor led to significant positive changes in blood pressure and heart rate variability, significantly improving VN activity. A 2009 study published in the Journal of Manipulative and Physiological Therapeutics yielded similar positive results for patients with lower back pain. Both of these studies concluded that the reduction in pain levels allowed patients to breathe slower and improve their vagus nerve function, and that chiropractic manipulation provided a positive effect on patients’ mechanical function. Especially when one is in pain, chiropractic care can be a very effective method of therapy and can have a significant benefit for VN and parasympathetic activity.
Electrical Stimulation
Over the past hundred or so years, researchers have conducted tests to learn about the effects of the vagus nerve. One technique involved stimulating the vagus using electrical stimulation devices on experimental animals. In addition to learning about the importance of the VN itself, researchers eventually determined that by electrically stimulating the vagus nerve, they were able to supplement its functions.
In the 1980s and early 1990s, experiments were done to show that stimulation of the vagus in the neck was effective in reducing seizure activity in dogs. This research led to dedicated clinical trials that produced vagus nerve stimulation (VNS) devices that could be implanted in the neck. These devices were approved by the FDA in 1997 for the treatment of epilepsy, and in 2005 for the treatment of chronic, treatment-resistant depression. Since that time, researchers and corporations have been producing and improving devices to electrically stimulate the VN for various medical conditions including headaches, bipolar disorder, treatment-resistant anxiety disorders, Alzheimer’s disease, and obesity. Today, the most common clinically used electrical VNS device is the NCP System from Cyberonics, which is implanted on the left vagus nerve during an outpatient procedure. This unit is used to treat patients dealing with severe treatment-resistant depression and/or epilepsy.
Right-side VNS is effective in animal models of epilepsy and seizures but is not known to have strong effects on depressive symptoms. Preliminary human trials are promising and have yielded positive effects, and some companies have already begun creating vagus nerve stimulation tools that can be used for various conditions. The CardioFit system from BioControl Medical uses right-side VNS to activate efferent fibers and aid in treatment of heart failure, while the FitNeSS System from BioControl Medical is designed to activate afferent fibers, thus helping to reduce side effects of electrical vagal stimulation.
Typical surgical risks associated with this procedure include infection, pain, scarring, difficulty swallowing, and vocal cord paralysis. Side effects from implanted electrical stimulation devices include voice changes, hoarseness, throat pain, cough, headache, chest pain, breathing problems (especially during exercise), difficulty swallowing, abdominal pain, nausea, tingling of the skin, insomnia, and bradycardia (slowing of the heart rate). Although many of these are temporary, they can be severe and can last permanently.
There are other devices for electrical stimulation that do not need to be implanted, though they show mixed results and are approved for certain conditions only at this point. The NEMOS system from Cerbomed is a transcutaneous VNS device that is applied to the part of the ear that is innervated by vagus. It has been cleared for treatment of epilepsy and depression in Europe at this time. The gammaCore device from US-based company electroCore has been granted clearance in Europe for acute treatment of cluster headaches, migraines, and medication overuse headaches. The gammaCore is a handheld portable device with two flat stimulation contact surfaces that are applied to the side of the neck over the vagus nerve. Larger trials are underway for treatment of other conditions.
As promising as electrical stimulation of the vagus nerve is, I would recommend using daily exercises and forming beneficial habits before trying external equipment such as electrical stimulation devices. If you are able to produce a strong effect on your vagus nerve activity using the exercises discussed previously, I feel the symptoms will improve drastically without unnecessary risks and costs.





