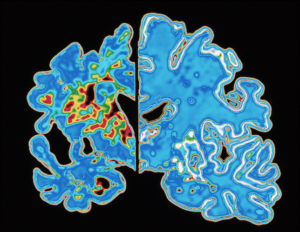
TO REVERSE ALZHEIMER’S, SEEK ITS TRIGGERS: AN INTERVIEW WITH DALE BREDESEN, MD
By Erik Goldman, Editor, Monday, 14 May 2018 14:56
Ronald Peters, MD …………..Commentary
In this landmark study Dr. Bredesen shows that Alzheimer’s Disease can be reversed by detoxifying the brain and body of toxins, such as environmental chemicals, mold and heavy metals (eg lead and mercury). This is a basic tenet of integrative or functional medicine, but it is unusual for this approach to be coming from UCLA Medical School, which has for decades received Big Pharma funding to continue the search for pharmaceuticals that mostly reduce the symptoms of chronic disease, but rarely cure it. Up to 60% of Americans have chronic disease such as heart disease, diabetes, arthritis and much more. Symptomatic medications create good business for the drug industry, but healing is better for patients.
 Those are bold statements, especially from a conventionally-trained neurologist. But Dale Bredesen, MD, is used to challenging orthodox views.
Those are bold statements, especially from a conventionally-trained neurologist. But Dale Bredesen, MD, is used to challenging orthodox views.
After more than 30 years of intensive research into the molecular mechanisms underlying Alzheimer’s (AD), and clinical experience caring for thousands of patients, Bredesen is convinced many of medicine’s central dogmas about dementia are misguided at best, flat-out wrong at worst.
“Despite the billions and billions of dollars spent by government agencies, pharmaceutical companies, and biotechnology wizards to invent and test drugs for Alzheimer’s, 99.6% of what we have come up with have been abysmal failures, not even making it out of the testing phase,” Bredesen writes in his stellar book, The End of Alzheimer’s (Avery 2017).
In most other diseases, science may be slow, but it is at least moving in the right direction, with significant gains to justify the massive expenditures. Not in Alzheimer’s.
Of 244 AD drugs tested between 2000 and 2010, only one—memantine–was approved. Its benefits are marginal. And beyond discovery of the ApoE gene, a major risk predictor, the genome revolution has not led to major advances either.
Practitioners and patients have become resigned to futility. Most see an AD diagnosis as a slow and unusually cruel death sentence.
Goodbye to the “Long Goodbye”
Bredesen, who is Director of the Mary S. Easton Center for Alzheimer’s Disease Research, at UCLA, as well as the Founding President and CEO of the Buck Institute—the nation’s first independent center for research on neurodegenerative disease—has a very different view.
“AD can be prevented, and in many cases its associated cognitive decline can be reversed. No one should die of Alzheimer’s,” Bredesen told Holistic Primary Care. Contrary to mainstream dogma, the agonizing “long goodbye” of dementia need not be inevitable.
He bases this hopeful message on a thorough understanding of the mechanisms that drive the disorder, and on years of successfully applying a holistic, personalized, lifestyle-based protocol in real-world settings.
He calls it the ReCODE protocol (Reversal of Cognitive Decline), and has spent the last few years developing algorithms to help practitioners evaluate myriad risk factors, and to tailor nutritional, botanical, lifestyle and in some cases, drugs, for each individual. Medication, he says, is the “dessert, not the main course” in his treatment approach.
The research that led to ReCODE began in 1989. Bredesen published his first paper on these protocols—then known as MEND (Metabolic Enhancement for Neurodegeneration) in 2014 in the journal, Aging. It quickly became one of the most-read papers in the journal’s history.
Rather than aproverbial silver bullet, ReCODE provides what he terms, “silver buckshot” targeting multiple factors that contribute to cognitive decline.
Identifying “Neuroterrorists”
Conventional medicine’s stunning lack of progress on AD results from its blind adherence to an incorrect belief that b-amyloid in the brain—a defining feature of AD—is the cause of the disorder, says Bredesen. For decades, almost all AD research has been focused on b-amyloid, much in the way cardiologists became single-minded about LDL cholesterol.
But more often than not, drugs aimed at b-amyloid either had either no meaningful effect on cognition (despite reducing plaque buildup), or paradoxically accelerated cognitive decline.
That’s because while b-amyloid does result in cognitive damage, it is not a primary cause of AD. Rather, it is an adaptive response to infectious, inflammatory, or environmental triggers.
Bredesen and colleagues have identified 36 key drivers—or “neuroterrorists”— in the pathogenesis of AD: These include:
- insulin resistance,
- diabetes, and
- obesity;
- gluten sensitivity;
- leaky gut;
- refined carbs;
- trans fats;
- chronic emotional stress;
- lack of exercise;
- nutrient-depleted diets;
- sleep problems;
- microbiome dysregulation;
- smoking;
- dental infections;
- exposure to environmental toxins;
- mycotoxins;
- infection with Borrellia (Lyme), Herpes, Babesia, and other common chronic infections.
Identify and address those triggers, and you can prevent or reverse the disease.
Housekeeping Gone Haywire
The condition we’ve named “Alzheimer’s” arises from a complex of chronic stressors that, in aggregate, shift the brain’s natural balance away from synapse creation and memory maintenance, and toward programmed neuronal death and memory pruning.
In a sense, it’s a neurological analog to the osteoblast-osteoclast balance in the bones. Under certain conditions the dynamic tension between these two opposed processes shifts to favor osteoclasis. The net result is osteoporosis.
In health, the brain maintains homeostasis between neuronal maintenance and neuronal destruction, between memory-preservation and memory-dissolution. Poor nutritional status, chronic viral and bacterial infections, environmental toxin exposures, genetic predispositions, and drug exposures can tip the balance to favor the latter. Over time, the result is dementia.
Like many disease states, Alzheimer’s arises when a natural and normal physiological housekeeping process goes haywire.
Bredesen has found that people with dementia not caused by stroke or head trauma tend to fall into one of three subtypes based on the predominant drivers:
- Type 1-Inflammatory (“Hot”): triggered by infection, inflammation-inducing diet, leaky gut, chronic insulin resistance
- Type 2-Atrophic (“Cold”): triggered by shortage of nutrients, hormones, and trophic factors that support neuronal function
- Type 3-Toxic (“Vile”): triggered by exposure to toxic metals, xenobiotics, or mycotoxins.
Insulin resistance is intimately connected to AD. It drives systemic inflammation, and indirectly leads to amyloid plaque buildup. Once insulin has transported glucose into cells, it is broken down by Insulin-degrading enzyme (IDE). But this enzyme is also responsible for breaking down b-amyloid in the brain. In conditions of excess insulin, the body preferentially shunts IDE toward insulin breakdown, meaning that b-amyloid accumulates.
Gluten sensitivity is another common factor. Over time, it leads to breaches in the barrier integrity of the gut wall, which means inflammation-inducing compounds from the intestinal lumen pass into the bloodstream. In advanced cases, this can lead to breaches of the blood brain barrier as well.
In reality most AD patients show complex combinations of factors. But typically, one set of drivers predominates. These become leverage points for clinical intervention.
The “Cognoscopy”
Dr. Bredesen recommends that all people over age 45 get a “cognoscopy.”
This is a set of blood tests for inflammatory markers, infections (especially Herpes simplex, Borrelia, P. gingivalis, and fungi), fasting insulin, thyroid and sex hormones, environmental toxins (especially heavy metals and mycotoxins), vitamin D, and gluten sensitivity, plus a comprehensive nutritional analysis, microbiome assessment, genome sequencing (especially for ApoE status), brain MRI with volumetric assessment, and cognitive performance tests (using an online system like BrainHQ).
By synthesizing this information, skilled clinicians can determine which of the many contributors predominate, and then work to eliminate the triggers, clear existing b-amyloid buildup, and finally rebuild and restore synapses.
The multifactorial, aggravated assault on the brain goes on for 15 to 20 years before someone notices symptoms that warrant medical attention. That means there is a very wide window for early intervention, says Bredesen.
What follows are excerpts of our extensive interview with Dr. Bredesen on April 30, 2018. We touched on the role of prescription drugs in triggering dementia, the risks and benefits of cannabis, the connection between depression and dementia, the benefits of ketogenic and gluten-free diets, and strategies for implementing ReCODE.
HPC: What would you say are the most important leverage points that primary care doctors can use for preventing or curing AD?
DB: First of all, we don’t ever say it is curable, because you need autopsies to show that. But we are reversing cognitive decline. For the people who have it, that means everything. That’s demonstrable, proven, and published in peer-reviewed journals. It happens all the time.
Primary care physicians are the most important physicians when it comes to dealing with the AD epidemic. According to new epidemiologic studies, it is now the 3rd leading cause of death. The claim has been there’s “nothing you can do about it.” We find differently. But you have to look at what is the underlying fundamental driver of the process.
When people just write a prescription, they are doing that without really knowing what’s causing the problem.
So we spent a lot of years looking at what actually gives you this disease. Yes, there are plaques and tangles, and the brain degenerates. But why? There’s a very short list of things that cause human disease: pathogens, toxins, metabolic changes, trauma, and genetics. That’s it.
If you look at larger data sets of Alzheimer’s patients, you see there are subtypes: Inflammatory, Glycotoxic, Atrophic, Toxic, Vascular, Traumatic.
So you can learn to look at people and see, “Oh, here’s a person whose primary problem is exposure to mycotoxins.” In another, the primary problem is rapid reduction in trophic support from estradiol, progesterone, vitamin D. Then you can address the things that are causing it. That’s when you get these striking improvements.
Primary care physicians see people long before neurologists do. They’re the ones who can evaluate these things and get them on appropriate treatments. Very few patients should ever have to go to a neurologist. In truth, there are not enough neurologists out there to handle the number of people with cognitive decline. The only reason it is working currently is because people aren’t coming in for care because they know there’s nothing that can be done.
There are 75 million Americans who are ApoE4-positive. If they were to flock in, they would overwhelm the neurological infrastructure. So this MUST be taken care of by primary care. And I think it is BEST taken care of by the primary integrative and holistic physicians.
HPC: In The End of Alzheimer’s you write about the issue of misguided pharmaceutical use. There have been a number of recent reports linking dementia with various classes of commonly used prescription drugs. How big is this “iatrogenic” piece of the AD risk puzzle?
DB: It is a very good question. An article just came out showing that once someone has a diagnosis of AD or dementia, they get put on all kinds of inappropriate drugs. Secondly, there are drugs that people use that are predisposing them to dementia. There’s no question it plays a role. In people we’re seeing, it probably plays a major role in 15%.
The majority of patients have toxin exposures, ApoE4 positivity, glycotoxicity, and inflammatory processes whether from leaky gut, poor diet, sleep apnea, or metabolic syndrome. Those are the big ones. But 15-20% have long-term use of antihistamines, antidepressants, benzodiazepines because of their GABA-ergic effect, drugs with anticholinergic activity.
A really common risk factor is multiple anesthesias. Repeated exposure to general anesthesia can be very damaging. Not only are there toxins on board, but you also have periods of hypoxia during general anesthesia.
HPC: What about opioids? Are they a risk factor?
DB: There doesn’t seem to be much of an association, though they’re dangerous for other reasons. It’s things that have anti-cholinergic effects that have the biggest negative impact on cognition.
HPC: Do stimulants like Adderall pose a risk? They’re widely prescribed, especially for children and young people.
DB: In colleges these days, everybody’s taking Adderall. We don’t know yet if it will increase problems in the future. But what we do know is you’re flogging your brain, so you could be causing damage that may come back to haunt you. It certainly looms as a future concern. A lot of people with early AD take Adderall to try to enhance their focus and memory. I try to get people off that when we can. If we address what’s actually causing the problems, they shouldn’t need Adderall.
 Brain networkHPC: There’s a lot of attention on cannabis and CBD these days. Many aging Baby Boomers have used cannabis for decades. Does it increase risk? Or on the other hand, can cannabis-derived substances play a beneficial role?
Brain networkHPC: There’s a lot of attention on cannabis and CBD these days. Many aging Baby Boomers have used cannabis for decades. Does it increase risk? Or on the other hand, can cannabis-derived substances play a beneficial role?
DB: We use CBD oil in the ReCODE protocol, especially for people who have trouble sleeping. It’s helpful and not a problem. As far as long-term use of THC, we recommend to try to minimize that. It can be problem, long-term, with memory storage. Just like everything else, use it in moderation. There’s some suggestion of a mild anti-AD effect from THC in cannabis. But we generally try to use cannabis without THC in the form of CBD oil.
HPC: According to your model, environmental toxins are implicated in the etiology of dementia. How big a factor is this?
DB: Have you seen Dr. Joseph Pizzorno’s recent book, The Toxin Solution? It goes into the things we are exposed to today, that our parents and grandparents were not exposed to. It is pretty striking. We are in a situation where we’re exposing ourselves to what I call “dementogens.” We should be aware of them, and should be able to able to protect ourselves from too much exposure.
I wrote a paper in 2016 that estimated there are at least 500,000 Americans who already have Alzheimer’s due to mycotoxins and other biotoxins, what I call Type 3 AD. That’s probably an underestimate.
Enjoying our content? Why not subscribe for access to our premium content?
Discover our online and print offerings here.
When I trained in the early 1980s, I’d never heard of anyone at age 49 or 51 or 53 developing AD, unless it was a dominantly inherited form, which is only 5% of all cases. Now, we’re seeing it almost every day, women typically around the time of menopause, coming in with this toxicity-associated AD. It is really concerning. I worry about that as a coming epidemic.
HPC: What’s driving that? Are the molds changing? Are our immune systems shot? Are we less able to handle the mycotoxins? Why predominately in women?
DB: We don’t know. It appears that what happens is, you live with this stuff and you sequester it in your bones, just like you do with mercury. Then at menopause, the osteoblastic to osteoclastic ratio changes, you start releasing it and you develop symptoms of AD. We’re seeing it commonly now.
And there have been changes in the molds, too. Dr. Ritchie Shoemaker (author of Surviving Mold) has suggested that just as bacteria have adapted to our use of antibiotics, the fungi have adapted to our use of fungicides. They share plasmids.
We see the Alzheimer’s part of this, but people also get asthma, rashes, chemical sensitivities, fibromyalgia or chronic fatigue. We think these are all different diseases, but they are all related to our response to toxins.
HPC: Ketosis seems to be an important part of ReCODE. In the book, you describe a diet called “Ketoflex 12/3,” with the 12 indicating the ideal number of hours between the last evening meal and the first morning meal, and the 3 representing the hours between the last meal and bedtime. Do you recommend that people stay in constant, mild ketosis, or is it more of an on-off regimen?
DB: Either constant or in cycles—you can cycle on and off once a week.
Most people who have AD have insulin resistance. Ed Goetzl at UCSF published some beautiful papers looking at neural exosomes in the blood. He looks specifically at a molecule called IRS-1 (Insulin Receptor Substrate). If IRS-1 is signaling from insulin, you have a high degree of tyrosine phosphorylation. But if IRS-1 is turned down, if it’s resistant, then you have serine and threonine phosphorylation. So he looks at this ratio and can tell if someone is insulin resistant or sensitive. He found that 100% of people with AD are insulin resistant.
Humans were not made to consume the amount of simple carbs that we now consume. The way we’re supposed to be living, you’d have occasional exposure to carbohydrates. But most of the time you’d be out foraging and hunting, and you’d be in and out of ketosis. You wouldn’t have access to a lot of sweets. We have 24/7 access.
So, from hundreds of papers, we know this is an important contributor to cognitive decline. Within the entire ReCODE protocol, we want to get people back to a diet very low in simple carbs. And then we want to replace that with ketones. We look for a low degree of ketosis, around 0.5-2.0 millimolar. But what we’ve been finding recently is that it works better if you get between 1.0 and 4.0. People on the higher side seem to do better than those on the lower side.
This is not a meat-based ketogenic diet, by the way. This is a plant-based, whole-foods ketogenic diet.
There are 3 ways to get into ketosis. Fasting and exercise, which is the best way. But people with low BMIs just cannot do this. The second way is to supplement with MCT (medium chain triglyceride) oils. The third is to supplement with exogenous ketones—ketone esters or ketone salts. Whichever way you do it is fine, if it gets your ketones up to a reasonable range to provide support that the brain needs without causing the insulin resistance.
HPC: Going gluten-free seems to be an important part of the ReCODE strategy. Is that a general recommendation for everybody, or only for those who prove gluten-sensitive on lab tests?
DB: If you don’t know whether you’re sensitive, then you should err on the side of going gluten-free. If you want to avoid that, get a Cyrex array 2 and 3 test, to make sure you are not gluten-sensitive. As Prof. Alessio Fasano has pointed out, most people are sensitive to gluten to some degree. I’m not talking about celiac disease. But most people will have issues with things like leaky gut due to gluten. So just get off it, unless you can truly show you’re not truly sensitive. Once you start leaking stuff into the bloodstream, you have an inflammatory state, and that fuels Alzheimer’s.
HPC: Does the microbiome play a role in all of this?
DB: Yes, absolutey. Part of it has to do with microbes associated with gut leak. But beyond that, there are microbiome profiles associated with insulin resistance, and obesity, and depression, and chronic inflammation. So part of this protocol is about prebiotics and probiotics. But only after we’ve made sure that the gut is healed. We want to make sure that we have a non-leaky gut first. Then we want to make sure we’ve optimized the microbiome.
HPC: You mentioned depression. Are people who experience depression and suicidality predisposed to dementia? Is there a connection between programmed cell death and “programmed self death?”
DB: Certainly there is a relationship between depression and AD. What we see from our side, looking at people with cognitive decline, is that the Type 3 AD is overwhelmingly associated with depression. The Type 1s and 2s do not often present with depression.
Type 3 very commonly starts with depression, because you have HPA axis dysfunction. Often these people get misdiagnosed with depression, and then later realize it is more than just depression. They’re actually becoming demented. They often have systemic inflammation, which is associated with depression. There are neurotransmitter changes associated with depression. So these things are intimately interconnected.
“Programmed self death” is an interesting term. We have had people who will simply not do the right things after we say, “Look, here’s what you have, and here’s what you can do to get better.” We had one woman who did improve after the first several months, and then she just said, “I don’t want to do this, I don’t want to do that.” When we got to the bottom of it, her granddaughter—her pride and joy–had left, gone away to college. The woman just wanted to die.
 HPC: Botanical medicines play a significant role in ReCODE. In the book you recommend a number of herbs including Ashwaghanda (500 mg twice daily) to CoffeeBerry Coffee berries reduce amyloid; Bacopa ( 250 mg twice daily) to raise cholinergic function; Gotu Kola (500 mg, twice daily) to improve focus, and several others that can be useful depending on what type of AD someone has. I’m particularly intrigued by whole fruit coffee extract (WFCE), aka “coffee berry.”
HPC: Botanical medicines play a significant role in ReCODE. In the book you recommend a number of herbs including Ashwaghanda (500 mg twice daily) to CoffeeBerry Coffee berries reduce amyloid; Bacopa ( 250 mg twice daily) to raise cholinergic function; Gotu Kola (500 mg, twice daily) to improve focus, and several others that can be useful depending on what type of AD someone has. I’m particularly intrigued by whole fruit coffee extract (WFCE), aka “coffee berry.”
DB: Whole fruit coffee extract is very promising. I learned about it from Dr. David Perlmutter. It increases brain-derived neurotrophic factor (BDNF), which is possibly the most important trophic factor for the brain, especially in cognitive decline. So we’re enthusiastic. We suggest it as part of the protocol. The molecular mechanisms have not yet been worked out. We don’t know how this is doing it but it clearly increases BDNF and seems to have a positive effect. So it’s a very nice thing to have.
In general we’re always looking for things that will help people. That’s one that seems to be very helpful.
HPC: ReCODE offers tremendous hope in a situation that most people reflexively see as hopeless. But it is quite complex. How do you plan to operationalize ReCODE, so it will be more widely accessible?
DB: This has definitely been a problem. As long as a doctor understands how to look for root causes and can spend enough time, people will do very well. But that is definitely a challenge.
So first, we train a network. We’ve now trained (through the Bredesen’s company, MPI Cognition, and the Institute for Functional Medicine) over 1,000 doctors from 10 different countries and all over US. And we’ve had over 2,000 patients on the protocol. These doctors learn and then continue to teach.
The second thing, in order to optimize care, we should all have access to computer-based algorithms that become our assistants. Just like you would have an intern, or a coordinator, or an LPN or RN, you should also have computer- based algorithms to optimize the evaluation and treatment of each complex chronic illness. This is not simple, that’s why these algorithms can be so helpful.
HPC: Have you already created algorithms for AD treatment?
DB: Yes. We call it the RECODE Report. It looks at 150 different inputs– different lab data, different ratios. It subtypes for you. So you can say, “This person is mainly an atrophic type, so I really need to optimize their trophic support.” Or, “This person is primarily a toxic type, and I need to look more closely at mycotoxins.” It will generate an initial (intervention) program. We’ve already generated algorithms for AD, and we’re now generating them for multiple other neurodegenerative diseases.
HPC: Do you envision someday a network of ReCODE clinics around the country, almost like a franchise model?
DB: Yes, absolutely. We’ve been approached by people who want to set up that sort of thing. So we are actively in discussions to do exactly that. Right now, there are already several hundred doctors who are using the protocol. We really want to optimize and simplify it, to make it accessible to everybody. The goal here is to reduce the global burden of dementia, and then extend this model to other neurodegenerative diseases, and ultimately to all chronic illnesses.
END





