TRENDS IN EARLY-ONSET CANCERS AMONGST YOUNG ADULTS
by Donald R. Yance, CN, MH | Jan 29, 2025
https://townsendletter.com/trends-in-early-onset-cancers-amongst-young-adults/
A growing body of research suggests that rates of early-onset cancers — those affecting patients younger than 50 years of age — have been rising since the 1990s. Studies have shown increasing rates of early-onset breast, lung, gastrointestinal, gynecologic, genitourinary, and hematologic cancers, among others.
In a recent 2023 study published in JAMA Network Open, researchers examined patterns in the incidence of early-onset cancers in the US from 2010 through 2019, based on data from the SEER 17 database. The authors identified 562,145 patients with early-onset cancer during the study period.
The results revealed an increase in the incidence of early-onset cancers — from 99.96 cases per 100,000 people in 2010 to 102.97 cases per 100,000 in 2019, for an annual percentage change (APC) of 0.28% (P =.01). At the same time, there was a reduction in the incidence of cancer for individuals aged 50 years and older (APC, -0.87%; P <.001).
“Overall trends show many of the cancers with the largest increases in early-onset disease are in the gastrointestinal tract, including cholangiocarcinoma, colorectal, gastric, appendix, and pancreatic cancers,” said Suneel D. Kamath, MD, of the Cleveland Clinic Taussig Cancer Institute in Ohio.
The greatest increase in early-onset cancers over the study period was seen for gastrointestinal cancers (APC, 2.16%; P <.001). In 2019, most early-onset cancers were breast cancer (n=12,649), followed by thyroid cancer (n=5869), and colorectal cancer (n=4097).
Over the past two to three decades, the incidence of early-onset colorectal cancer has increased at a rate of 1-2% per year. Mortality rates have also increased by 1% per year, according to a 2024 American Cancer Society report.
Patients between the ages of 20 and 49 that are diagnosed with colorectal cancer have larger and faster-growing tumors as well often already metastasized compared to older adults.
The increasing rates of early-onset colorectal cancer “are not due to an increase in germline-syndrome related cancers, as 70% of these cancers are sporadic in younger patients, so there is clearly some environmental exposure(s) that may be a driver,” Dr Kamath noted.

The increasing incidence of early-onset cancers is expected to continue for the near future, said William M. Grady, MD, of Fred Hutchinson Cancer Center in Seattle, Washington.
However, researchers have suggested that lifestyle changes and reducing exposures to environmental carcinogens could help lower rates of early-onset cancers. Implementing cancer screening at younger ages and modifying treatment approaches could improve outcomes for patients who do develop early-onset cancers.
In another 2023 study, published in BMJ Oncology, researchers found a 79.1% increase in the global incidence of early-onset cancer and a 27.7% increase in the number of related deaths between 1990 and 2019.2
A 3rd recent study, published in the journal Lancet Public Health, in July 2024, found that Generation X, millennials in US have higher risk of developing 17 cancers compared to older generations.
For certain cancers, people born in 1990 face two-to-three times the risks that those born in 1955 did.
“Researchers with the American Cancer Society (ACS) assessed rates of 34 different cancers among those born between 1920 and 1990, based on how many were diagnosed with or died of the disease from 2000 to 2019.
On average, the rates of 17 types of cancer, including pancreatic, breast and gastric cancer, have risen with each new generation since 1920, the study found. Previous ACS research had shown that rates of 11 cancers, including pancreatic, colorectal, kidney, uterine and testicular cancer, had been increasing among young adults. The new study added eight more types of cancer to that list:
- Gastric cardia cancer (a cancer of the stomach lining)
- Cancer of the small intestine
- Estrogen receptor-positive breast cancer
- Ovarian cancer
- Liver and bile duct cancer
- Non-HPV-associated oral and pharynx cancer (only in women)
- Anal cancer (only in men)
- Kaposi sarcoma (a cancer of the blood vessel lining and lymph nodes, only in men)
Rates doubled or even tripled for some of these cancers, including kidney, pancreatic and small intestine cancers, in people of either gender. For women, liver cancer incidence has increased two- to threefold since the 1920s. Even cancers that seemed to be in decline for baby boomers and other older generations — including some breast cancers and testicular cancer — are now a greater risk again to millennials and Gen X-ers, the study found.
More young people are dying of some of these cancers as well; mortality from colorectal, gallbladder, testicular and uterine cancers has increased over the generations, as has the fatality rate of liver cancer, but only for women.”
In another new study researchers from Brigham and Women’s Hospital saw that more and more people under the age of 50 are being diagnosed with cancer of the breast, colon, esophagus, kidney, liver, pancreas and more — globally — in a trend that took a sharp upward turn around the year 1990.
“From our data, we observed something called the birth cohort effect. This effect shows that each successive group of people born at a later time (e.g., decade-later) have a higher risk of developing cancer later in life, likely due to risk factors they were exposed to at a young age,” said Dr. Shuji Ogino, professor of pathology and physician-scientist at Brigham and Women’s, in a press release.
“We found that this risk is increasing with each generation,” Ogino continued. “For instance, people born in 1960 experienced higher cancer risk before they turn 50 than people born in 1950 and we predict that this risk level will continue to climb in successive generations.”
Americans are also dying of heart failure today at a higher rate than they did in 1999, reversing years of progress in reducing the death rate.
That is the stark message of a new JAMA Cardiology study, which finds that the current mortality rate from heart failure is 3% higher than it was 25 years ago. Based on data from death certificates, the study says, the mortality rate fell significantly from 1999 to 2009, then plateaued for a few years before sharply increasing from 2012 to 2019. During the pandemic years of 2020 and 2021, the latest year for which data is available, heart failure deaths accelerated.
What is causing the sudden rise and cancer and actual heart failure as well?
Several factors may be driving the increase in early-onset cancers, Dr Grady noted. He said these factors include “increasing rates of obesity, decreasing physical activity, increasing incidence and younger age of onset of adult-onset diabetes mellitus, increased exposure to chemicals in plastics and microplastics, poor sleep hygiene, and dietary changes such as increased consumption of ultra-processed foods and refined sugars and decreased consumption of whole foods.”6,7
In the BMJ Oncology study, for example, researchers identified dietary factors — such as a diet high in red meat and sodium and low in fruit, whole grains, and calcium — as well as alcohol and tobacco use as the main risk factors for early-onset cancer.2
Researchers from Ohio State University presented at the recent American Society of Clinical Oncology conference in Chicago found signs that a high-fat, low-fiber diet may increase inflammation in the gut that prevents it from naturally suppressing tumors. The cells of young people with colorectal cancer also appeared to have aged more quickly — by 15 years on average — than a person’s actual age. That’s unusual, because older people with colorectal cancer don’t have the same boost in cellular aging.
This latest research has linked a bacteria called Fusobacterium to colorectal cancer. It’s not unusual for fusobacterium to be present in a person’s mouth, but it is more likely to be found in the intestines of colorectal cancer patients, compared to healthy people. One study even found that people with colorectal cancer were five times more likely to have fusobacterium in their stool compared to healthy people.
Researchers analyzed data from UK Biobank participants who were recruited between 2006 and 2010 and were followed up to February 2022. They evaluated associations between early-life factors and early-onset CRC risk overall, focusing on long-term and recurrent antibiotic use. The team also estimated associations between long-term and recurrent antibiotic use in early life and CRC risk by polygenic risk score using 127 CRC-related genetic variants, as well as a particular gut microbiota regulatory gene, Fusobacterium (FUT2). Associations for early-onset colorectal adenomas, as precursor to CRC, were also evaluated. The study included 113,256 participants. There were 165 early-onset CRC cases and 719 early-onset adenoma cases.
Increase in the numbers of middle-aged people dying of stroke
In recent years, many more middle-aged adults between the ages of 45 and 64 have been dying from strokes, according to a new report from the Centers for Disease Control and Prevention (CDC).
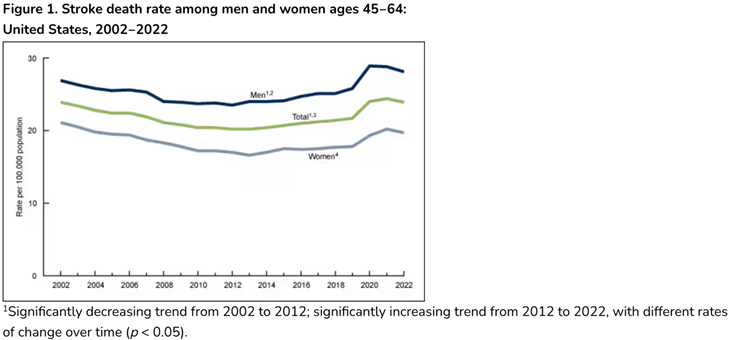
“After declining from 2002 to 2012, stroke death rates for middle-aged adults increased 7% between 2012 and 2019, and increased an additional 12% through 2021, the CDC found. The stroke death rate then fell slightly (by 2%) for men through 2022, and “did not change significantly” for women.”
One contributing factor might be the overuse of antibiotics
Mounting evidence suggests that microbiota dysbiosis caused by antibiotic administration is a risk factor for serval cancers, including CRC, as well as breast cancer.
“The findings suggest that individuals with genetic risk factors (ie, family history of CRC) who have experienced early-life antibiotics use on a long-term basis are probably at increased early-onset CRC risk,” the authors concluded. “Given that antibiotics remain valuable in the management of bacterial infections during early life, investigating the pros and cons of early-life antibiotic use is of great significance.”
Some data has linked long-term or recurrent antibiotic use in early life to an increased risk of early-onset colorectal cancer via alterations in the gut microbiome.8
Triple-negative breast cancer patients who used antibiotics within three years of diagnosis have an increased risk of death, according to a study. The gut microbiome is a likely link.
A 2019 systematic review and meta-analysis of observational studies that assessed the association between antibiotic use found that prolonged use of antibiotics with a small increased risk of various cancers throughout a lifetime.
Antibiotics not only act on bacteria that cause infections but also affect the resident microbiota. The observation that the gut microbiome can be permanently perturbed even by short-term or low-dose antibiotic treatment, and that this change can have long-term effects on health, cautions against widespread and potentially unnecessary use of antibiotics, particularly in young children and pregnant women, and illustrates that antibiotics should not be considered harmless.
Obese individuals exhibit marked differences in the composition of the intestinal microbial community as compared to lean subjects. These changes in the gut microbiota precede the clinical manifestation of overweight. antibiotic-induced changes in the gut microbiota influence host metabolism and lead to fat accumulation. The intestinal microbiota perturbation caused by antibiotic exposure in the perinatal period appears to program the host to an obesity-prone metabolic phenotype, which persists after the antibiotics have been discontinued and the gut microbiota has recovered.
Emerging evidence indicates that disruption of the intestinal flora play an important role in the pathogenesis of depression. As one of the causes of such disturbances, the role of antibiotics in depression risk is gradually being revealed.
Antibiotics up to 6 months before immune checkpoint inhibitor therapy reduced overall survival and progression-free survival across multiple malignancies, according to a study presented at the Virtual 35th Annual Meeting of the Society of Immunotherapy of Cancer.
There is also a relationship between antibiotics and chemotherapy efficiency. Antibiotic administration appears to be associated with reduced efficacy of neoadjuvant therapy and poor prognosis in breast cancer patients.
Antibiotics, which were previous believed not to negatively impact the immune system now have been associated with major dysregulation of the innate immune defense system.
Obesity, Leptin and Some Natural Compounds to the Recue
Overall increases in obesity, for sure, is one contributing factor that accounts for around 5%. According to a recent study published in JAMA Oncology, that involved 85,000 women, being overweight increases the risk of early-onset colorectal cancer by 37%, while obesity increases the risk by 93%, almost doubling it. Dr. Kortmansky explained that obesity alters hormone levels, specifically the hormone leptin promotes tumor growth, and is a potent driver of cancer stem cells., This, in turn, triggers the early onset of other cancers, such as breast, pancreatic, and endometrial cancers. Many studies have demonstrated that elevated chronic serum concentrations of leptin, frequently seen in obese subjects, represent a stimulatory signal for tumor growth.
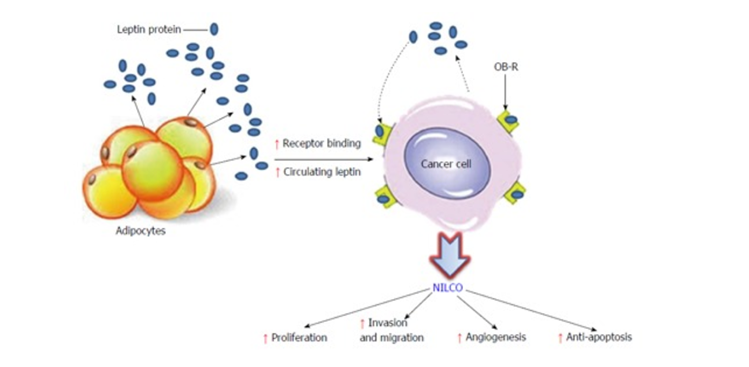
Obesity, leptin, Notch, interleukin-1 and leptin crosstalk outcome, and cancer progression.
Natural compounds that have shown to suppress tumor growth through leptin inhibition
Isothiocyanates, which are compounds within edible cruciferous vegetables inhibit oncogenic actions of leptin in human breast cancer cells by suppressing activation of signal transducer and activator of transcription 3.
Honokiol, an active compound in Magnolia bark (Magnolia grandiflora) extract, has shown to abrogate leptin-induced tumor progression. Honokiol significantly inhibits leptin-induced breast-cancer cell-growth, invasion, migration and leptin-induced breast-tumor-xenograft growth.
Vitamin D suppresses leptin stimulation of cancer growth through microRNA. hTERT (human telomerase reverse transcriptase), downregulation is a key event mediating the anti-leptin activity of 1,25(OH) vitamin D in estrogen-sensitive tumors in women.
Conjugated linoleic acids (CLA), has shown to decrease fat and increase lean mass in several animal studies. CLA is found predominately in “ORGANIC” milk fat from free-range grass feed cows. CLA promotes weight loss, while retaining lean muscle mass. It appears to reduce body fat, improve insulin sensitivity and lower leptin levels.,
Reggiano parmesan cheese, one of my favorite foods in the world, is very rich in CLA.
Dietary intake of seaweeds is associated with a lower prevalence of chronic diseases. While seaweeds are of high nutritious value, due to their high content of fiber, polyunsaturated fatty acids and minerals, they also contain an abundance of bioactive compounds. These bioactive compounds include peptides, polyphenols (phlorotannins and bromophenols), polysaccharides (alginate, fucoidans, laminarin), carotenoids (fucoxanthin), and phytosterols, abundant in Undaria pinnatifida (Sea Mustard, Miyeok, Wakame), Saccharina japonica (formerly Laminaria japonica; Kelp, Dasima, Kombu), and Saccharina latissima (Sugar kelp). Although seaweed products show promising preventive and therapeutic effects of seaweed products, it is crucial to consider potential health risks.
In a study taken place on the Chinese population, people who took CLA supplements for 12 weeks lost more body fat and inches off their waistlines than those who didn’t take the supplements. But some other sources suggested a modest benefit in weight loss.
Recently, many studies have presented the anti-obesity effects of brown seaweeds and their secondary metabolites, such as phlorotannins. However, studies that target the appetite hormone leptin are few. In this study, we explored the natural anti-obesity agents from brown seaweeds targeting leptin. Also, we investigated the anti-obesity effects of ishophloroglucin A.
Ishophloroglucin A favorably docks to the leptin receptor. Ishophloroglucin A reduced body weight and food intake in C57BL/6J-ob/ob mice. Ishophloroglucin A stimulated the leptin and the insulin signaling.
What about the COVID-19 Vaccines?
There is a lot of speculation around the S Protein from both the COVID-19 vaccines, as well as chronic COVID-19, which involves an ongoing state of inflammation and immune weakness/vulnerability.
In a review published on Dec. 26, 2023, the authors of a study, found non-live vaccines tend to increase a person’s risks of all-cause mortality. The researchers found that non-live vaccines such as influenza, COVID-19, hepatitis B, and diphtheria-tetanus-pertussis tend to cause adverse nonspecific effects (NSEs), increasing a person’s risks of all-cause mortality and infections from other diseases.
In the case of COVID-19 vaccines, live vaccines were likely not considered due to concerns about the formation of recombinant viruses when a vaccinated person comes into contact with the circulating viral strain.
The COVID-19 vaccines may be associated with adverse events, increased inflammation and immunological stress, because of the presence of highly toxic spike proteins, which studies now link to long COVID and vaccine injuries.
How might the microRNA vaccines disrupt the normal response of the immune orchestra?
According to a (June, 2022) published paper in Food Chem Toxicol, states the following: “Immune cells that have taken up the vaccine nanoparticles release into circulation large numbers of exosomes containing spike protein along with critical microRNAs that induce a signaling response in recipient cells at distant sites. We also identify potential profound disturbances in regulatory control of protein synthesis and cancer surveillance. These disturbances potentially have a causal link to neurodegenerative disease, myocarditis, immune thrombocytopenia, Bell’s palsy, liver disease, impaired adaptive immunity, impaired DNA damage response and tumorigenesis.”
However, the same could be said about the virus itself, especially in those with long COVID. For me the argument is less about the vaccine risk-to-benefit ratio, and more about the crime of not sharing the very good news and overwhelming data on the beneficial effects of herbal medicine, nutritional medicine, and dietary medicine, which very clearly has demonstrated to reduces the onset of COVID-29, the duration and severity, the hospitalization, and duration in the hospital and the reduction of death from COVID-19. This is the real crime. Because of this coverup I cannot believe or trust anything that the establishment tells us to be true and in the best interest of our health.
Increased Age-Adjusted Cancer Mortality After the Third mRNA-Lipid Nanoparticle Vaccine Dose During the COVID-19 Pandemic in Japan
During the COVID-19 pandemic, excess deaths including cancer have become a concern in Japan, which has a rapidly aging population. Thus, this study aimed to evaluate how age-adjusted mortality rates (AMRs) for different types of cancer in Japan changed during the COVID-19 pandemic (2020-2022). Official statistics from Japan were used to compare observed annual and monthly AMRs with predicted rates based on pre-pandemic (2010-2019) figures using logistic regression analysis. No significant excess mortality was observed during the first year of the pandemic (2020). However, some excess cancer mortalities were observed in 2021 after mass vaccination with the first and second vaccine doses, and significant excess mortalities were observed for all cancers and some specific types of cancer (including ovarian cancer, leukemia, prostate cancer, lip/oral/pharyngeal cancer, pancreatic cancer, and breast cancer) after mass vaccination with the third dose in 2022. AMRs for the four cancers with the most deaths (lung, colorectal, stomach, and liver) showed a decreasing trend until the first year of the pandemic in 2020, but the rate of decrease slowed in 2021 and 2022.
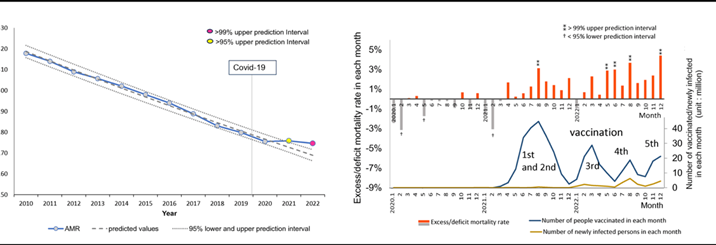
Age-adjusted mortality rates (AMRs) over time and excess mortality in each month: all cancers.
Almost 50% of the global disease burden is estimated to be associated with modifiable risk factors. Why isn’t there more of a moment to improve people’s lives by health optimization, utilizing diet, lifestyle, herbal, nutritional modalities to improve the lives of everyone and reduce the risk of cancer and other chronic diseases.
For example, a recent meta-analysis study found that a mediterranean diet reduced cardiovascular disease and mortality in diabetes. Another recent study, that included 41,243 participants, found that diet rich in fruits, vegetables, and legumes intake was associated with a significant reduced risk of all-cause, cardiovascular, and cancer mortality.
At the foundation of the Mederi-Care approach to health and healing, is a focus on nourishing the root system, where we enhance and optimize robustness, auto-regulation, and auto-organization, at the molecular, cellular and organ system levels. Mederi-Care utilizes a body of practices, procedures, and systems, that together forms the Mederi-Care methodology.
Author
Donnie Yance is a master herbalist and certified nutritionist with over 30 years of experience. He is the founder of the Mederi Center for Natural Healing, specializing in integrative cancer care and chronic illness. Donnie’s expertise combines traditional healing systems with modern science to support overall health and vitality.

