YOUR INTERNAL ARMY – PROTECTING YOU FROM INFECTION AND CANCER
 These fearless internal warriors are a part of you. They are cells in your immune system. Macrophages, cytotoxic T-cells, natural killer cells and others protect you against infection from bacteria, viruses, and fungi. They also keep you from developing cancer by killing cells that have mutated and become renegade cells that can develop into full-blown cancer.
These fearless internal warriors are a part of you. They are cells in your immune system. Macrophages, cytotoxic T-cells, natural killer cells and others protect you against infection from bacteria, viruses, and fungi. They also keep you from developing cancer by killing cells that have mutated and become renegade cells that can develop into full-blown cancer.
You have trillions of these dedicated cells patrolling every recess of your body. They have only one goal – to protect you from disease.
You control your immune system and you do so everyday whether you know it or not. You are controlling your immune system when you choose what foods to eat, how much to worry, and how much stress you have on a daily basis.
We live in a stressful and complex society that creates many opportunities for us to weaken our immune systems and make us vulnerable to illness. Our food, water and air have toxins that buildup gradually in our bodies and can compromise our immune systems, mutate our DNA and further increase our susceptibility to disease.
It is up to you to understand and strengthen your immune system if you want to stay healthy. The following is an explanation of how your immune system works, as well as some guidelines for making this vital and protective system stronger, thereby protecting you from infections, cancer and many other health problems.
Membranes
 We live in a sea of bacteria, fungi, viruses and parasites. We cannot see them but they are everywhere. No matter how clean you think your skin, hair, nose, mouth, fingernails and other parts of you are, they have microorganisms on them.
We live in a sea of bacteria, fungi, viruses and parasites. We cannot see them but they are everywhere. No matter how clean you think your skin, hair, nose, mouth, fingernails and other parts of you are, they have microorganisms on them.
The sweat on your skin provides enough nutrients to support an average of 65,000 bacteria for every square inch of your body. Your intestines have three to five pounds of bacteria and fungi and most of them are beneficial to your health. Bacteria, viruses and fungi are entering your body daily in the foods, water and air that you consume.
Microbiologists estimate that there are more microorganisms in and on your body that there are cells in your body.
Your first line of defense against infection from these potential invaders is your skin and mucous membranes, which serve as barriers to keep them out of your body. The mucous membranes are the soft, skin like lining of your mouth, nose, airways, digestive tract and reproductive organs that secrete mucous. The mucous in your nose and airways, for example, is like flypaper which traps dust, fungus spores, pollen grains, bacteria, viruses and yeast cells from your inhaled air and transports them to the throat where they can be swallowed and killed in the hydrochloric acid of your stomach.
In addition to serving as physical barriers, your mucous membranes have other mechanisms to prevent microbial invasion. For example, tears and saliva contain lysozyme, an antibacterial enzyme that helps to destroy potential invaders. Also, mucosal secretions in your mouth, eyes, nose and entire digestive tract contain IgA antibodies, which are designed to bind to potential invaders and prevent their entry into your body. We will look at this important contribution to mucosal defense later on.
Your digestive tract has a big role to play in preventing infection and supporting your immune system. First of all, it has an immense surface area. Your bowels are about twenty feet in length, but the small intestinal surface is covered with tiny finger-like projections called villi that absorb nutrients from the foods you eat and keep out toxins and microbial invaders.
If the small intestine had a smooth inner surface, instead of all the villi, it would be two and one half miles long. This huge surface area combined with the intense exposure to foreign invaders, toxins and other immune stimulating antigens, makes the intestinal tract the largest organ of immune surveillance and response in the body.
One of the most important protective factors in the intestines is the bacteria population that lives there. Over 500 species of bacteria, weighing some three to four pounds, live in the healthy human bowels. In addition to augmenting your first line of defense against infection, they help your body in other ways as well.
 The normal microflora in the colon ferment soluble fiber to yield short chain fatty acids which supply 5 to 10% of human energy requirements. Healthy bacteria also synthesize at least seven essential nutrients, including folic acid, biotin, pantothenic acid, riboflavin, pyridoxine, cobalamin and vitamin K. They also participate in the metabolism and elimination of chemicals, including drugs, hormones and carcinogens.
The normal microflora in the colon ferment soluble fiber to yield short chain fatty acids which supply 5 to 10% of human energy requirements. Healthy bacteria also synthesize at least seven essential nutrients, including folic acid, biotin, pantothenic acid, riboflavin, pyridoxine, cobalamin and vitamin K. They also participate in the metabolism and elimination of chemicals, including drugs, hormones and carcinogens.
In terms of immune function, healthy bacteria in the bowel help to prevent infection in several ways. For example, a species of strep viridans commonly found in the intestines produces bacteriocin, a natural antibiotic that kills certain types of foreign bacteria. Healthy bacteria also produce toxic short-chained fatty acids that discourage foreign invaders. They also interfere with adherence of invading organisms and their sheer populations provide no place for new organisms to attach and grow.
The substantial benefits of healthy intestinal flora depend on the many species existing in a natural balance or ecology. Any environment in nature works best if all the species are present in a natural balance. If the balance is upset, then problems develop.
The same thing occurs in the digestive tract. If the natural ecology of organisms is upset, then a variety of health problems can develop. One of the most significant disturbances in the gut that weakens the immune system is increased intestinal permeability, or leaky gut syndrome. This is a condition, which allows large intestinal molecules from foods and other organisms to enter the body and challenge the immune system.
The following issues are known to increase bowel wall permeability.
- Recurrent or prolong use of antibiotics for any purpose also kill healthy bacteria which causes yeast organism, such as Candida albicans, to overgrow. Fungal overgrowth is very common in our society. The yeast organisms infiltrate the villi and disturb their function, thereby increasing permeability to unwanted factors.
- Non-steroidal anti-inflammatory drugs like Motrin disturb the bowel wall.
- The consistent consumption of alcohol and sugar further enhances yeast overgrowth.
- The ingestion of allergenic foods, like dairy, wheat and corn can irritate the bowel wall.
- Reduced stomach acidity can impair the digestion of proteins causing large molecules to exist further down in the intestines.
- Inadequate production of digestive enzymes by the pancreas also causes large molecules to float down and irritate the bowel wall.
- Bacterial and parasitic infections can irritate the bowel wall and weaken the immune system.
- Weak adrenal glands due to chronic stress can disturb bowel immunity and further disturb the natural ecology of the bowel.
- Cortisone-like drugs such as Prednisone suppress intestinal immune function and increase the likelihood of yeast overgrowth.
In summary, there are many common conditions that disturb bowel ecology, alter the permeability of the intestinal wall and weaken your first line of defense. The following is a list of symptoms associated with increased intestinal permeability.
- Fatigue and malaise
- Joint pain
- Muscle pain
- Fevers of unknown origin
- Food intolerances
- Abdominal pain
- Abdominal distention, gas and bloating
- Diarrhea
- Skin rashes
- Toxic feelings
- Disturbances in concentration
- Memory defects
- Shortness of breath and poor exercise tolerance
Supplements that support the first line of defense:
- Vitamin A
- L-glutamine
- N-acetyl-cysteine
- Probiotics
For these and many other reasons, your first line of defense may fail to protect you from infection. That is why the mindbody wisdom has the innate immune system.
Your Second Line of Defense: the Innate Immune System
Your second line of defense against infection is your innate immune system, which consists of phagocytes, natural killer cells and the complement system. These vigilant cellular warriors confront any organism that penetrates through your skin or mucous membranes and gains access to the interior of your body.
The innate immune system is the infantry of the immune system and it serves us very well because it is immediately ready for action and it has powerful resources.
Imagine getting a splinter in your finger, which allows just one bacterium to enter into your tissues. Bacteria can multiply very quickly. Scientists estimate that one bacterium can double in number every 30 minutes. This would give rise to 100 trillion organisms in one day! That is about how many cells you have in your entire body.
The volume of these 100 trillion organisms would be about 100 liters. You have about 5 to 6 liters of blood in your body. So it is easy to see that a few bacteria could wreak havoc in your body if you did not have the phagocytes, natural killer cells and complement system ready for action in every corner and recess of your body.
The cells of the innate immune system do more than just attack, eat and repel invaders. They also have receptors on their outer walls that can detect common microorganisms such as bacteria, viruses, fungi and parasites. This minute, molecular antennae pick up proteins from common invaders and display them to the cells of the adaptive immune system, thereby instructing them in where and how to join in the battle.
Phagocytes: Professional Killers
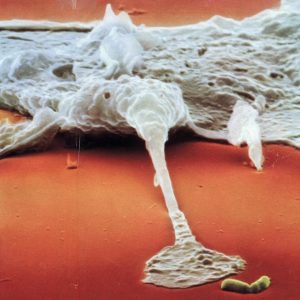
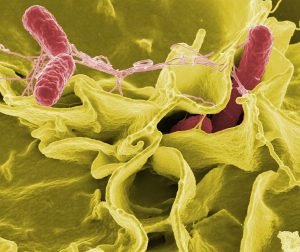
 Phagocytes are a variety of immune cells that have the ability to engulf, digest and thereby destroy invading microorganisms. Once a phagocytic cell ingests a microbe, it is isolated within a small spherical sac called a phagolysosome, which contains powerful enzymes, which break down the invader in to chemical components. This process is called phagocytosis.
Phagocytes are a variety of immune cells that have the ability to engulf, digest and thereby destroy invading microorganisms. Once a phagocytic cell ingests a microbe, it is isolated within a small spherical sac called a phagolysosome, which contains powerful enzymes, which break down the invader in to chemical components. This process is called phagocytosis.
Phagocytes also release chemicals called pyrogens, which serve to increase body temperature (fever) which further slows down and retards the growth of the invaders. Phagocytes not only eat viruses and bacteria, but they also eat aging cells of the body and clean up cellular and other debris found in the tissues.
Phagocytes are divided into two categories: granulocytes and monocytes.
There are three types of granulocytes, neutrophils, eosinophils and basophils. Neutrophils are discussed in another section. Eosinophils are few in number and they are involved in allergic reactions and protection against parasites. Basophils are involved in the early process of inflammation. Once they migrate into affected tissue, they are called mast cells.
Monocytes are the largest white blood cell. They comprise two to four percent of the circulating white blood cells. When they migrate into the tissues, they become larger and become the powerful macrophage, where they can live for months.
Substances that support phagocytes:
- Echinacea
- Progesterone
- Probiotics
- Vitamin E
Neutrophils
Neutrophils are white blood cells that serve as important phagocytes, or garbage collectors. There are about 100 billion of these cells produced every day in the bone marrow and they account for about 70% of the white blood cells in circulation in your body.
There are so many them made because they live only about five days before they undergo apoptosis or programmed cell death. They are professional killers that leave the blood vessels and enter the tissues of the body. As they leave the blood stream, they become activated for attack on any invader in your body.
Neutrophils do not recognize antigens on their victims like macrophages do, but they are voracious killers. If they find a bacterium, they engulf or ingest it into their bodies. Inside the neutrophil there is a whole battery of powerful chemicals that digest the invader into biochemical soup. The pus you see at an infected wound or splinter is mainly dead neutrophils that have sacrificed themselves to protect you from infection. Once the battle is over, chemical signals tell the neutrophils to revert back to their resting state where they continue to collect garbage.
Neutrophils are swept along in the blood stream at high-speed – about 1000 microns per second. In order for them to exit the blood vessel they have specialized adhesion molecules on their surface (called selectin ligands) that grab adhesion molecules on the surface of the endothelial cells that line the blood vessels. Quite a nifty system for escaping from the rapid flow of blood.
Neutrophils are activated by a variety of cytokines, or chemical messengers, in the tissues. These cytokines draw the neutrophils to an area where infection may be occurring, such as a splinter in your toe. The neutrophils in turn release other cytokines, which create the inflammation that you experience as redness and tenderness around the infection. Inflammation serves to obstruct bacteria from invading your tissues any further. Once the neutrophils and other immune cells have finished off the invaders, the inflammation subsides and the immune cells quietly return to their normal patrols.
Macrophages
Like neutrophils, macrophages are powerful phagocytes. Macrophage means “big eaters”. In their resting state they too are garbage collectors that rid the body of cellular debris. Unlike neutrophils, however, they are more specialized in their defensive capabilities and they live for months in the body.
Macrophages are made in the bone marrow from stem cells, like all other blood cells. When newborn macrophages leave the bone marrow and enter the blood stream, they are called monocytes. You have about two billion of these “young macrophages” in your blood at any one time. The monocytes circulate in the blood for about three days. When they find an escape route through the cells that line the capillaries, they leave the blood and enter the tissues where they mature into macrophages.
During their patrols of the body, they can become activated by cytokines that an infection may be occurring. In response to the message, they rush to the site of invasion and it is there that they do something that neutrophils cannot do. As they engulf bacteria or viruses, they display fragments of the invader’s protein on their cell surfaces, like little molecular flags. These protein fragments are called antigens.
When other immune cells, like cytotoxic T-cells, recognize the foreign antigens, they become activated in turn and help to mount a more vigorous immune response. Therefore, in their primed state, macrophages are excellent antigen presenters for the rest of the immune system. In other words, they are sentinels that patrol the tissues of the body looking for invaders and prepared to not only attack directly, but also to signal other immune cells to move in and assist in the battle.
Macrophages also secrete numerous cytokines to orchestrate the immune system. One of these cytokines is tumor necrosis factor (TNF). TNF is a molecule that can kill cancer cells and virus-infected cells directly. The activated macrophage increases its production of TNF by producing more lysosomes within its body. A lysosome is a tiny structure within the macrophage that produces powerful chemicals and enzymes that are designed to kill invaders.
In addition, macrophages can produce hydrogen peroxide, which helps to kill invaders. Macrophages can kill much larger parasites by engulfing a part of the parasite and then dumping its lysosome full of toxic chemicals into the invader.
So macrophages are versatile cells that can serve as garbage collectors, antigen presenters and vicious killers.
Supplements and nutrients that enhance macrophage activity:
- Aloe Maitake
- Astragalus Modified citrus pectin
- Beta-1,3-glucan Muramyl polysaccaride-glycan complex
- Berberine Olive leaf extract
- Cordyceps Probiotics
- Coriolus versicolor L-glutamine
- Echinacea Zinc
- Enzymes Coenzyme Q10
Natural Killer Cells
Natural killer cells (NK cells) are unique in the immune system forces. Scientists are not sure where they come from and where they mature in the body. They are probably in the same family as lymphocytes, but they share characteristics with macrophages.
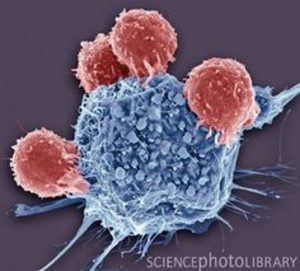
Natural killer cells are versatile once they enter the tissues and begin their patrols of the body. These powerful and deadly cells look for and kill cancer cells, virus-infected cells, bacteria, parasites and fungi. NK cells have two known methods for killing unwanted cells.
First, they can bore a hole in a target cell by secreting a protein molecule called perforin. Their second method of attack and destroy is unique. They secrete a protein called Fas ligand, which interacts with a surface protein on the target cell called Fas.
When these two connect they create a signal they travels to the nucleus of the bacteria, virus-infected cell, or cancer cell and tells the cell to commit suicide, a process called apoptosis by immunologists. These alternative killing methods make NK cells one of the most potent protectors in the immune arsenal.
How do they know which cells to kill and which ones to leave alone? This has been a mystery for immunologists. T cells recognize foreign invaders because they have receptors on their surfaces that recognize foreign material, ie anything that is not you. But NK cells do not similar receptor sites.
It appears that they look for MHC 1 molecules on any cell they approach. MHC stands for major histocompatability complex. These large molecules are on every cell in your body and they identify a cell as part of you. When transplant surgeons look for donator organs, they match MHC molecules between the recipient and the donor. So the NK cell simply kills when there no MHC molecule to be found on the suspicious cell and backs off when it recognizes MHC signals that the cell is “one of us”.
MHCs are like little antennae on every cell in your body signaling that this cell is part of the family. They also have another unique ability. Once a cell is infected with a virus, fragments of the virus are carried to the surface of the cell where they are attached to the MHC molecule like a flag on the flagpole. This is the signal that a virus is inside the cell. NK cells and cytotoxic T-cells read the message and begin the attack.
NK cells are very important to your defense against cancer and other viral diseases. Their activity is low with chronic fatigue syndrome and certain nutritional deficiencies. Low NK cell activity is also a risk factor for developing cancer. These cells, like others in the immune system can be activated by proper nutrition, stress reduction and nutrients. It is important to be aware of your NK cells in order to keep your immune system working at optimal levels.
There are laboratory tests to measure the number of natural killer cells in your blood. More importantly you can determine natural killer cell cytotoxic activity levels in laboratory tests as well. It is one thing to know how many NK cells are circulating in your blood, but it is far more important to know how vigorously they can function. Natural killer cell activity is the best single measure of immune strength and can be used to monitor the success of cancer prevention and treatment.
Supplements and nutrients that enhance natural killer cell activity:
- AHCC Modified citrus pectin
- Ambrotose Siberian ginseng
- Aloe Thymus extracts
- Andrographis panniculata Thymic protein A
- Astragalus Vitamin C
- Flavinoids Vitamin K3
- Coriolus versicolor Essential fatty acids
- Enzymes Organic germanium (GE-3)
- Garlic N-acetyl-cysteine
- IP-6 DHEA
- MGN-3
The Complement System
The complement system is the name given to a complex series of about 20 proteins which can work together to destroy invaders and signal other immune cells that an attack is occurring. It is an important part of the innate immune system, along with phagocytes and natural killer cells.
The proteins that make up the complement system are produced in the liver. They are then released into the blood where they circulate and move into the tissues of the body. The most abundant complement protein is called C3.
Under normal circumstances, C3 molecules circulate in the blood and tissues and are frequently cut into two smaller proteins, C3a and C3b. C3b is a highly reactive and short lived molecule that from a molecular perspective is like a tiny “bomb” that does one of two things. If it is very close to a bacterium, it will bind to the outer wall of the invader. If there is no cell wall to attach to, it will neutralize itself and disappear by binding with a water molecule. If it binds to the outer surface of a bacterium, it will stabilize there waiting for the next step in complement activity. Another complement protein, B will bind with C3b and complement protein D will then clip off part of B to yield C3bBb.
Now the process gets interesting. Now imagine a single bacterial cell with C3bBb glued to its cell surface. C3bBb is now an enzyme called C3bBb convertase, which will clip other C3 molecules into more C3b, which will also attach to the outer wall of the bacterial cell. Now the bacterium is covered with C3bBb “decorations,” each of which will now clip another complement protein, C5, producing C5b. C5b will now in turn combine with other complement proteins (C6, C7, C8 and C9) to form a “membrane attack complex” or MAC for short.
Now, the targeted bacterial cell has a “stalk” of complement proteins attached to its outer wall and C9 proteins are finally added that “saws” a tiny hole in the surface of the bacterium. Now the bacterium dies as its cellular contents pour into the environment, rather like being shot with a gun. The whole process is an incredible molecular blast that happens very quickly leaving the invader to spill its guts and die. Macrophages and other phagocytic cells will then move in and clean up the mess.
This complement killing process is similar to the way that cytotoxic T cells kill cells that are infected with virus. These cells use a protein called perforin to bore a hole in the targeted cell wall. Well, C9 is very much like perforin.
Since these tiny MACs bombs are going off all over the place, you may wonder why they don’t attach to the cells of your own body. The wisdom of the body has safeguards to prevent this from happening. Firstly, there is a protein on the surface on the cells of your body called decay accelerating factor, or DAF, which causes a breakdown of C3bBb, thereby preventing this process from damaging your own cells. Secondly, there is another protein on healthy cells called CD59, which can kick nearly complete MACs off the cell surface before they drill a hole.
In summary, the proteins of the complement system are present in high concentrations in the blood and tissues of your body and they are ready to attack any invader that is around with this high-speed process. There are other ways that complement can be activated to do its invader destroying work, but you get the picture of how powerful and effective this protective mechanism really is.
The complement system has other functions in addition to producing membrane attack complexes. Once C3b attaches to an invader, it can be clipped by another protein into iC3b, which inactivates the C3b from producing more MACs. However iC3b attracts phagocytic cells, like macrophages, because the phagocytes have complement receptors on their cell surface that bind with iC3b and enhances their cell gobbling activity. Also, other fragments of the complement cascade serve as chemical attractants to recruit other cells of the immune system to join in the battle.
So you can see that the complement system is a powerful protective process that not only kills invading cells directly, but also attracts and activates phagocytes to join in the fight.
Supplements that enhance complement function:
- Beta-1,3-glucan
- Vitamin C
Your Third Line of Defense: the Adaptive Immune System
Many animals do just fine with physical barriers to infection and an ever-ready innate immune system. However, for the higher organisms, like you and I and most animals with backbones, the creative intelligence of the universe (a.k.a. Mother Nature) created a third line of defense – the adaptive immune system.
The adaptive immune system is based on specialized white blood cells called lymphocytes, which respond to microbial invasion in a powerful and unique manner. Lymphocytes called helper T cells recognize particles of invaders, or antigens, and then mobilize other lymphocytes, called B cells to make antibodies against the invader. Often macrophages that have already plunged into the battle will present an antigen to the T cells thereby activating them to join the fight.
It may take a week or two for the B cells to make specific antibodies for the battle at hand. That is why the innate immune system is so important in starting immune defenses immediately. Again, the innate immune system is the infantry waiting for attack, while the adaptive immune system is like the air force, which provides missiles, called antibodies, to assist in the defense.
Most scientists believe that the adaptive immune system evolved in order to protect us from viruses, which are difficult for the innate immune system to handle alone.
The adaptive immune system not only creates specific antibodies for an invader, it also has special cells, called memory B cells, that remember how to make that antibody at any time in the future if exposed to the same attack. This is the mechanism for immunization. Once the body has seen a fragment of an invader, it will ready itself to make antibodies against the invader and then remember how to do so in the future.
T-cells
T cells are lymphocytes that are “born” in the bone marrow from stem cells. There are about a trillion of these important cells circulating in your blood at any one time. Eventually they travel to the thymus gland located in your chest, just beneath the breastbone. In the thymus gland they undergo a mysterious maturation process that enables them to recognize antigens in your body. An antigen is a protein fragment from a source outside of your body, usually a virus.
All T cells have T cell receptors (TCR) on their cell surfaces. TCRs are like little antennae, which can recognize a foreign antigen. Once a T cell picks up a specific type of antigen it will then undergo a clonal proliferation producing millions of T cells that are specifically designed to battle that particular antigen.
It is believed that the creative intelligence of the human body created T cells in order to combat viruses. While antibodies are capable of detecting invaders that are outside of your cells, viruses enter a cell where they cannot be found by antibodies. Once a virus is inside one of your cells it can take over the DNA reproduction process and thereby make millions of new viruses, which burst forth, starting the infectious process all over again. T cells recognize that a cell is infected with a virus by detecting a viral antigen on the surface of the infected cell and they begin reproducing in order to fight the virus.
There are three types of T cells: helper T cells, suppressor T cells and cytotoxic T cells.
Supplements that enhance T cell function:
- AHCC Vitamin B6
- Astragalus Vitamin C
- Beta-1,3-glucan Vitamin E
- Flavinoids Organic germanium (GE-3)
- Cordyceps Conjugated linoleic acid
- Echinacea L-arginine
- Enzymes L-glutamine
- MGN-3 N-acetyl-cysteine
- Muramyl polysaccaride-glycan complex Selenium
- Siberian ginseng Glutathione
- Thymus extracts DHEA
- Vitamin A
Helper T-cells
Helper T cells are the quarterbacks of the immune team because they secrete cytokines that activate and coordinate other immune cells in the battle against viral attack. There are many different cytokines, each with a specific purpose in coordinating immune resistance to infection.
Once activated by the recognition of a viral antigen, helper T cells secrete cytokines, including interferon gamma, interleukin-2, and tumor necrosis factor.
Interferon gamma activates macrophages and influences B cells to make antibodies against the viral invader. Interleukin-2 is a growth factor that stimulates natural killer cells and cytotoxic T cells to proliferate and join in the attack. And, tumor necrosis factor also activates macrophages and cytotoxic T cells.
Supplements that enhance helper T cell function:
- Sterols and sterolins
- Thymus extracts
- Thymic protein A
- Melatonin
Suppressor T-cells
The immune system is activated by helper T cells to fight any viral invader. After the virus is eliminated by the coordinated action of numerous immune cells, suppressor T cells secrete cytokines that turn off the immune activation.
Interleukin-10 acts to decrease the proliferation of helper T cells, while interleukin-4 causes macrophages to stop releasing interleukin-12 and tumor necrosis factor. In this manner, the activated immune system returns to its normal function of patrolling the cellular environment looking for other invaders.
While doctors measure suppressor T cell numbers and activity in immune diseases, there is substantial debate amongst research immunologists as to whether or not there is a special suppressor T cell type. Nonetheless, T cells are capable of activating the immune system and, in turn, turning in off once the battle is finished.
Cytotoxic T-Cells
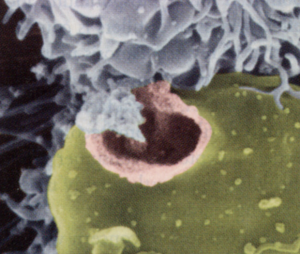
Cytotoxic T cells (also called killer T cells and cytotoxic lymphocytes) are a special weapon in the immune arsenal. Like all T cells, they originate in the bone marrow and then travel to the thymus gland where they mature into powerful virus killing cells.
Like all T cells, they have T cell receptors on their surface that can recognize viral protein particles. They recognize viral protein, or antigen, when other immune cells present it, such as macrophages.
Cytotoxic T cells proliferate under the influence of interleukin-2, which is secreted by helper T cells. Once activated, they seek viral infected cells and close in for the kill.
Cytotoxic T cells exert their deadly influence on virus infected cells in two ways. The first is by secreting a protein called perforin. Perforin literally bores holes in the cell wall of the infected cell, thereby disrupting cell function and the cell dies, a process called necrosis.
The second killing method occurs when the cytotoxic T cell dumps and enzyme called granzyme B into the infected cell. Once inside the target cell, granzyme B triggers the cell to commit suicide, or apoptosis. Apoptosis involves destruction of the infected cell’s DNA by the cells own enzymes. Since viruses attach to DNA, the virus is destroyed also.
Supplements that enhance cytotoxic T cell function:
- Aloe
- Maitake
- Vitamin K3
- Zinc
Dendritic Cells
 Dendritic cells are similar to macrophages in that they have the ability to present antigen to naïve T-cells, thereby activating them for battle. Dendritic cells live in various tissues of the body where they look for foreign proteins, or antigens.
Dendritic cells are similar to macrophages in that they have the ability to present antigen to naïve T-cells, thereby activating them for battle. Dendritic cells live in various tissues of the body where they look for foreign proteins, or antigens.
These cells are very effective in collecting antigens from the fluid in the spaces between cells in the body. They can process four times their own volume of fluid in one hour, thereby collecting antigens for presentation to T-cells. As they collect antigen, they mature, settle down and connect with other dendritic cells by extending branch-like appendages to each other. They look like starfish connected to each other.
In addition to activating T-cells, dendritic cells can secrete interleukin-2, interleukin-4 and gamma interferon in order to further mobilize a specific immune response.
Dendritic cells are especially important in the defense against cancer. While they do not attack cancer cells directly, they are very effective at looking for molecular structures on the surface of cells that signify cancerous activity. In other words, they seek out tumor specific antigens and present these to cancer killing cytotoxic T-cells.
Medical scientists believe that dendritic cells can trigger a potent anti-cancer attack. Researchers around the world are looking for dendritic cell vaccines. Several trials are ongoing at the present time and preliminary results are very encouraging. In one trial, a 16 year old girl with metastatic fibrosarcoma, previously treated with chemotherapy, showed striking regression of all metastatic activity after three weeks of therapy.
In these research trials, dendritic cells are isolated from the patient, stimulated to grow in numbers and then exposed to tumor antigens. The antigen-loaded cells are then injected back into the patient in order to boost the cancer killing activity of the healthy immune system.
While dendritic cell vaccines are very effective in animal studies, there is a lot of controversy about what antigens to use in activating the isolated dendritic cells.
Supplements that enhance dendritic cell function:
Muramyl polysaccarihe-glycan complex
Antigens
Antigens are the molecules, usually proteins that are found in microorganisms such as bacteria, viruses and parasites. Once an antigen enters the body, it is confronted by a variety of lymphocytes all bearing antibodies. Once an antibody is found that binds specifically with an antigen, then the lymphocyte proliferates and becomes an antibody producing plasma cell. Each plasma cell secretes only one antibody, which is specific for the particular antigen.
B Cells, Plasma Cells and Memory Cells.
While macrophages, neutrophils, and natural killer cells are the infantry of the immune system, forever patrolling the inner recesses of your body looking for invaders, B cells provide the air force with its arsenal of missiles, called antibodies that are specifically designed to target invaders who have escaped the infantry. Like all other blood cells, B cells are born in the bone marrow from stem cells. Immunologists estimate that approximately 1 billion B cells are made each day of your life.
A primary distinguishing feature of B cells is that while they are developing in the bone marrow, they create from the genetic code, a B cell receptor that is displayed on their outer surface. The B cell receptor is anchored to the outer wall of the B cell by a protein sequence, which serves as a footing for the molecule. Antibodies, which are produced by the B cell later in its life, are identical to the B cell receptor, except for the anchoring protein sequence. Therefore, antibodies made by the B cell simply leave the molecule and travel in the body as part of the immune response.
Each B cell produces only one specific antibody against one specific antigen, or foreign protein from an invading microorganism or some other allergic substance. Also each B cell has a B cell receptor that is unique to the kind of antibody produced by that particular cell. How B cells make so many antibodies against all of the possible viruses, bacteria, parasites and other foreign proteins such as inhalant allergens is one of the many remarkable aspects of mindbody wisdom in general and the immune system specifically.
This is how the tiny B cell receptor on the surface of the B cell works. If an antigenic protein, say from a bacterium, fits into the B cell receptor, and if a cluster of B cell receptors are filled with antigen, then a signal is sent to the nucleus of the B cell to begin making antibodies for that antigen. Antibodies then pour from the cell to attach to the invader, tagging it for attack by other immune cells.
B cells that have just emerged from the bone marrow and have never produced antibodies are called “naïve” by immunologists. For naïve B cells to be activated there is another step required. In addition to the specific antigen being recognized by the B cell receptors on the young cells surface, a helper T cell must make contact with the surface of the B cell, providing a co-stimulatory message that is sent to the nucleus of the B cell. Once both signals are present, certain sequences of DNA in the nucleus begin to produce just the right antibody for the problem at hand.
Once a B cell has been activated by T cell stimulation, then it develops a mysterious cellular memory for the antigen. In the future, if it comes across that antigen again, it will activate and produce antibodies without the need for T cell stimulation. This is the memory mechanism that provides for the effectiveness of immunization.
Also, when B cells have been activated they create new proteins on their cell surface which are receptor sites for interleukin-2, a cytokine that acts as a growth stimulator that causes B cells to proliferate and pour out antibodies when they are needed. Again, the release of interleukin-2 comes from helper T cells, the quarterbacks of the immune system who call the immune defense into action.
Once a B cell has been activated by T cells and specific antigen recognition, it then has a career choice. It can become a plasma cell or a memory cell. If it becomes a plasma cell, it can produce two thousand antibodies per second! Think about that for a moment, two thousand per second. You didn’t know how powerful you are at the cellular level did you? Such prodigious activity cannot last long however, as the plasma B cell will live for only a few days.
The other career choice for B cells is to become a memory cell and this is very important to long term immune function. The memory B cell remembers the first exposure to an invading antigen, occurring either naturally as with infection or a designed exposure as with immunization. Memory B cells develop high affinity B cell receptors on their surfaces so that even tiny amounts of specific antigen can be detected, leading immediately to antibody production.
Supplements that enhance B cell function:
- Colostrum
- Vitamin B6
- Vitamin C
- Organic germanium (GE-3)
- L-arginine
Mast Cells
Mast cells are white blood cells that protect us against parasitic infection. They contain large numbers of tiny sacs of granules, each filled with powerful chemicals. The best known of these chemicals is histamine, which is involved in allergic reactions. When a mast cell encounters a parasite, it dumps its chemicals onto the invader in order to kill it. The release of chemicals is called degranulation.
Mast cell degranulation also occurs as part of an allergic reaction, such as the stuffy, runny nose and eyes associated with inhaled pollens. Usually mast cells release their chemicals in a small area of the body, producing allergic symptoms such as allergic rhinitis or asthma. But these chemicals are powerful and if a large number of mast cells empty their granules at one time, the allergic reaction can be severe enough to be life threatening. This is called anaphylaxis and occurs, for example, when a bee stings highly sensitive people.
Mast cells have sensitive receptor sites for IgE antibody on their outer walls. When enough of these sites are filled with IgE, the mast cell is like a tiny hand grenade, waiting to explode. At some critical point, the mast cell receptor sites signal the cell to dump its potent chemicals into the local surrounding environment.
Antibodies
 Antibodies are proteins that have a special structure designed to bind to antigens. There are five classes of antibodies: IgG, IgA, IgD, IgE and IgM. IgG makes up about 75% of the antibodies in blood. All antibodies are made by B cells, which are white blood cells that originate in the bone marrow. Once a B cell matures into an antibody factory, it is called a plasma cell.
Antibodies are proteins that have a special structure designed to bind to antigens. There are five classes of antibodies: IgG, IgA, IgD, IgE and IgM. IgG makes up about 75% of the antibodies in blood. All antibodies are made by B cells, which are white blood cells that originate in the bone marrow. Once a B cell matures into an antibody factory, it is called a plasma cell.
One of the many marvels of the immune system is the diversity of antibody production. In order to protect us from the astronomical number of possible infections from viruses, bacteria, parasites, as well as a variety of allergenic inhalants and foods that we are susceptible to in our complex world, immunologists estimate that we need about 100 million different antibodies.
Since each B cell makes only one antibody, how does the body know how to create so many on demand? Susumu Tonegawa solved this riddle in 1977 and his work earned him the Nobel Prize. The answer is based on changes that occur in antibody genes, modular design of antibodies and a type of mix and match strategy, which is rather complicated. Suffice it to say the cells of your immune system are expert in making these ingenious little molecules. Once again, the mindbody wisdom that orchestrates the movement of molecules and cells in your body is working to create life for you.
Antibodies serve their vital role in immune defense by attaching to an antigen thereby marking it for death. The antibody doesn’t do the killing itself, but simply becomes a tag identifying the invader for attack from other immune cells. Imagine a single bacterial cell with antibodies hanging all over its outer surface, rather like ornaments on a Christmas tree. But these ornaments are deadly decorations as macrophages and other phagocytic cells are now drawn to the bacterium preparing to eat it.
Antibodies also attach to viruses, but the process is a little different here. In order for viruses to gain entry into one of your cells, they must bind to receptor molecules on the cell surface. These receptor molecules are designed for cellular communication, among other things, but the virus has learned to use these sites for its own purposes.
Once inside a cell the virus attaches itself to the DNA and redirects the reproductive machinery to make copies of itself, i.e. more viruses. But once again, the immune system is prepared for such invasive tactics. Plasma cells make antibodies that attach to the part of the virus that plugs into the receptor site on the cell surface, thereby preventing the virus from docking on the surface of the cell. These are called “neutralizing antibodies”. As a result, the virus is forced to remain outside of your cells where it becomes a meal for macrophages and other phagocytes.
As I mentioned, there are four main classes of antibodies: IgM, IgA, IgG and IgE. When antibody producing B cells are first activated they produce IgM antibodies. IgM antibodies are made from five IgG antibodies stuck together into one large complex.
IgM antibodies tend to stay in the blood stream and are very effective at killing bacteria that have entered the blood stream from a wound or some other route. They appear early in an infection and their primary purpose is to activate the complement cascade. When IgM binds to a microbial invader it initiates a series of events that brings complement into action.
Complement is composed of about twenty different proteins that work together to destroy invaders and signal other immune cells that an invasion is taking place. IgM antibodies are also the neutralizing antibodies that bind to viruses, thereby preventing them from entering healthy cells in your body.
IgA antibodies are sentinels that serve the important task of guarding the mucous membranes in your body. Mucous membranes are soft, skin-like mucous secreting layers that line your mouth, digestive tract, eyes, nose, airways and reproductive organs.
There are about 400 square meters of mucosa in your body. These surfaces are a prime entry for bacteria, viruses and parasites that are in food, water and the air that we breathe. While microbes can easily enter your body in this way, they are immediately confronted with the IgA antibody as a first line of immune defense. Therefore, the body makes more IgA antibodies than all the other types combined. IgA antibody is found in secretions from the mucous membranes, such as tears, saliva, nasal fluids, sweat, colostrum and secretions of the lung, urinary and digestive tracts.
IgA antibodies are two IgG antibodies stuck together. This allows them to bind to microbes more efficiently. The IgA tagged bacteria and viruses clump together and are swept out of the body with the mucous. This is why a viral respiratory infection causes so much sneezing, coughing and watery eyes. Your body is ejecting viruses bound together by IgA antibodies and caught up in the mucous.
IgA antibody deficiency is very common. It can be measured in the saliva or the blood using simply and inexpensive laboratory tests. When this important antibody is low in the intestinal mucous membranes, there is reduced resistance to harmful microbes, such as bacteria and parasites. When these abnormal organisms grow in the bowel, there can be a variety of digestive symptoms, including loose stools, gas, bloating, and constipation. When the bowel population is severely disturbed by atypical and pathogenic organisms, the intestinal wall can become more permeable to proteins found in the bowel.
Proteins from foods, as well as yeast and bacteria can “leak” through the bowel wall and enter the blood stream. Antibodies in the blood then combine with the foreign protein, or antigen, creating immune complexes that must be cleared from the blood circulation. Clearing immune complexes creates inflammation that can affect any organ in the body, producing a variety of symptoms, such as muscle and joint pain, headache, fatigue, rashes, impaired concentration and a foggy feeling in the mind. This common problem has been called “leaky bowel syndrome”. Psychological stress is a common cause of reduced IgA production.
IgG antibodies are also called gamma globulin, which is given to people exposed to infections such as hepatitis. Giving a shot of gamma globulin simply provides the body with more antibodies during a time of exposure and additional need for protection.
IgG antibody is a major workhorse in immune defense. It is an abundant antibody with a powerful ability to leave the blood circulation and diffuse deeply into the body tissues where it can neutralize bacterial invaders and toxins by tagging them for phagocytosis. IgG is unique among antibodies in that it can cross the placenta from the mother into the child growing in her womb. This provides major immune defense for the newborn in the first few weeks of his/her life.
There are subclasses of IgG antibody. IgG1 is used to bind to microorganisms, thereby targeting the invader for phagocytic immune cells to come in and finish the job. Macrophages and other phagocytes have receptor sites on their cell surfaces that bind directly to IgG1 so the tagged microbe is more easily found and destroyed. IgG3 antibody activates complement better than any other subset of IgG. Natural killer cells have receptor sites on their cell surfaces that bind to IgG3, thus stimulating the NK cells to locate and kill invading organisms more effectively.
IgE antibodies are uniquely powerful in their ability to trigger acute inflammatory reactions. When an invading infectious organism has penetrated beyond the IgA defenses, it will combine with IgE, which is located on the surface of mast cells, and thereby trigger the release of a host of chemicals, such as histamine. These chemicals create the inflammation that is seen with allergic reactions, producing symptoms such as runny nose and watery eyes.
On occasion, when a toxin spreads throughout the body, the mast cell chemical release can be severe and extensive, producing life-threatening anaphylaxis. For some sensitive people, a bee sting can initiate this severe form of IgE meditated allergic reaction.
Mast cells are white blood cells that contain lots of granules, or little sacks of chemicals, such as histamine, cytokines and other inflammatory mediators. Mast cells protect us from parasites by unloading their granules of toxic chemicals right onto the parasite in order to kill it. Because IgE can trigger potent inflammatory defense against invaders, very little is found circulating in the blood.
The final class of antibodies is IgD, which is not found very much in the blood. Most of the IgD is found together with IgM on the surface of a certain type of B lymphocyte. Immunologists believe that the two antibodies work together as antigen receptors for the control of lymphocyte activation and suppression.
Antibodies are powerful weapons in the defense against infections and invasion. They are produced by B cells that are told what antibody to make under the influence of helper T cells which “quarterback” the immune system. Helper T cells arrive at the site of a microbial invasion and then release cytokines, which tell the B cells what type of antibody to make for each type of invader – virus, bacterium or parasite.
B cells can become plasma cells, which are antibody-producing factories, or, they can become memory B cells which remember how to produce an antibody for a lifetime. This phenomenal ability is what makes immunization effective at protecting you against infections. If an antigen from polio of tetanus is introduced into your body through a vaccination, the B cells create antibodies to defend against the infection. Memory B cells remember how to make the antibodies so that if you are ever infected with a wild polio virus or infected with tetanus toxin, the memory B cells jump into antibody production based on their memory of how to do so. In this way you are given a jump-start in the battle against infection.
Supplements that enhance antibody production:
- Progesterone
- Vitamin A
- Vitamin B6
- Vitamin C
- Conjugated linoleic acid
- Selenium
- Coenzyme Q10
Cytokines: Chemical Messengers of the Immune System
 Cytokines are short-lived messenger molecules used for communication between cells of the immune system. These remarkable little molecules relay information between various types of immune cells, thereby coordinating and focusing immune response to infection or invasion.
Cytokines are short-lived messenger molecules used for communication between cells of the immune system. These remarkable little molecules relay information between various types of immune cells, thereby coordinating and focusing immune response to infection or invasion.
Hormones are chemical messengers that are sent from your endocrine glands, such as thyroid and pituitary, which direct and coordinate activities in the organs of your body. The third chemical communication system in the body is the neurotransmitters, which relay information between your brain and the rest of your body.
Cytokines, hormones and neurotransmitters provide an extensive internal communication network that organizes and coordinates events in your body. This is how your thoughts, emotions and stresses influence the events in your body, including your immune system. The communication between systems also overlaps, as nerves have cytokine receptors, just as immune cells can listen to neurotransmitters. This is why the immune system can be suppressed under times of stress.
Unlike hormones, which circulate in the blood for some time, cytokines often exert their influence in local tissues and only for a very short time. They are extremely powerful chemical messengers that communicate to other cells at low concentrations. Most immune cells have sensitive receptor sites that pick up the message from the short-lived cytokines. Receptor sites are like little antennae on the cell that receive specific cytokines like a lock fits into a key. If the key fits, the cell receives the message and acts accordingly. If the key does not fit the lock, then no message is delivered.
If a bacterial or viral invader is found in your tissues, the biochemical phone lines are buzzing with communication as to how to mount the best defense. As the coordinated attack proceeds between immune cells, cytokines are busy moving from cell to cell. Once the invader has been killed, then other cytokines down-regulate the immune system back into its baseline vigilance.
If you get a cut in your finger, cytokines organize the immune attack against any bacteria that may have entered through the wound, while other cytokines direct the process of inflammation and wound healing.
Immunologists are discovering more and more of these incredible messenger molecules and the cells that originate them and the cells that respond to their message. Our understanding of immune communication is by no means complete. So far cytokines are divided into at least five general categories: interleukins, colony stimulating factors, tumor necrosis factors, interferons and chemokines.
Interleukins
Interleukin-1 (IL-1): released by activated macrophages to stimulate resting T cells and B cells. IL-1 stimulates other cytokines to up regulate the immune system and stimulates the hypothalamus in the brain to produce a fever in response to infection.
Interleukin-2 (IL-2): released by helper T cells to produce proliferation of T cells and activation of cytotoxic T cells and natural killer cells.
Interleukin-3 (IL-3): released by activated T cells to support the growth of stem cells in the bone marrow as well as the growth of mast cells.
Interleukin-4 (IL-4): released by activated T cells to stimulate the production of activated B cells. (IL-4 was originally called B cell growth factor) IL-4 also stimulates the proliferation of resting T cells and mast cells, as well as stimulating cytotoxic T cells.
Interleukin-5 (IL-5): released by helper T cells and mast cells to stimulate natural killer cells, eosinophils, T cell activity and increase the production of IgA antibody.
Interleukin-6 (IL-6): released by helper T cells, macrophages, mast cells and other cells to induce the differentiation of activated B cells into antibody-secreting plasma cells. (IL-6 was originally called B cell differentiation factor) Also causes the liver to produce acute inflammatory proteins.
Interleukin-7 (IL-7): released by bone marrow cells to activate and direct T cells.
Interleukin-8 (IL-8): released by monocytes to direct and activate neutrophils.
Interleukin-9 (IL-9): released by T cells to produce growth and proliferation of other T cells.
Interleukin-10 (IL-10): released by helper T cells and macrophages to inhibit gamma interferon and aspects of cellular inflammation.
Interleukin-11 (IL-11): released by bone marrow cells to influence inflammatory reactions.
Interleukin-12 (IL-12): released by monocytes and macrophages to induce an immune enhancing subset of helper T cells.
Interleukin-13 (IL-13): released by T cells to inhibit inflammation and induce proliferation of B cells.
Interleukin-15 (IL-15): released by macrophages and other immune cells to activate natural killer cells and induce proliferation of T cells.
Interleukin-16 (IL-16): released by helper and suppressor T cells to influence cellular movement.
Interleukin-18 (IL-18): released by macrophages to influence natural killer cells and T cells as well as to increase gamma interferon.
Colony Stimulating Factors
Colony stimulating factors are cytokines that are necessary for the production of blood cells in the bone marrow. They provide a means for regulating and fine tuning bone marrow production in response to immune stimulation.
Interleukin-7 mentioned above is produced in the bone marrow in order to stimulate survival and growth of immature precursors to the B and T lymphocytes.
Stem cell factor is produced in the bone marrow in order to make bone marrow stem cells responsive to other colony stimulating factors.
Interleukin-3 is produced by helper T cells to act on all immature bone marrow cells that will differentiate into all known mature cell types.
Granulocyte-macrophage colony stimulating factor (GM-CSF): released by activated T cells, macrophages, and bone marrow cells in increase production of inflammatory white blood cells. It also activates macrophages.
Monocyte colony stimulating factor (M-CSF) and Granulocyte colony stimulating factor (G-CSF): produced by activated T cells, macrophages and bone marrow cells to increase production of inflammatory leukocytes.
Tumor Necrosis Factor (tnf)
Tumor necrosis factor is a cytokine released by activated macrophages that kills some cancer cells, stimulates the production of other cytokines and is capable of causing systemic reactions, such as fever, when in high enough concentrations. TNF also has anti-viral and anti-parasitic activity.
Interferons
The interferons were discovered in 1957, becoming the first cytokines to be identified. There are three types of interferon, alpha, beta and gamma. They are released by macrophages and T cells early on in response to infection, and are the body’s first line of defense against viruses. They stimulate natural killer cells to kill cells in the body that are infected with viruses and they make uninfected cells more resistant to viral infection.
Supplements that enhance and support cytokine production:
- AHCC Transfer factors
- Ambrotose Probiotics
- Beta-1,3-glucan Vitamin B6
- Flavinoids Vitamin C
- Lactoferrin Vitamin E
- Colostrum Essential fatty acids
- Echinacea Organic germanium (GE-3)
- Enzymes Magnesium
- Maitake Conjugated linoleic acid
- Sterols and sterolins Selenium
- Thymus extracts Zinc
- Thymic protein A
The Thymus Gland: Controller of Immunity
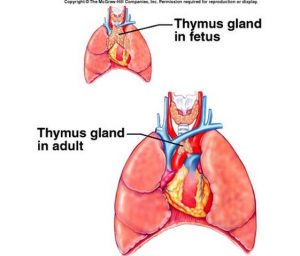 The thymus gland is a small organ that is essential to the proper functioning of your immune system. It lies in the front of your chest just behind the breastbone. It weighs about one third to one ounce at birth and reaches its peak weight of about 17 ounces at puberty.
The thymus gland is a small organ that is essential to the proper functioning of your immune system. It lies in the front of your chest just behind the breastbone. It weighs about one third to one ounce at birth and reaches its peak weight of about 17 ounces at puberty.
Thereafter, under the influence of many factors, including the adrenal stress hormones (go to how stress affects the immune system) like cortisol, as well as sex hormone, the active thymus glands begins to shrink in size and die off. Prescription steroid medications, like Prednisone, also cause the gland to wither and shrink. The gland is also extremely vulnerable to free radicals and oxidative damage caused by stress, radiation, infection and chronic illness. As the gland shrivels, fat and connective tissue replace the active thymus tissue. Much of the healthy thymus gland structure usually atrophies by age twenty and the decline accelerates throughout life.
Immunologists consider the shrinkage of the thymus gland as one of the cardinal biological markers of the aging process. In spite of its gradual loss of size, extensive research over the past 50 years has shown that the thymus gland is the key regulator of immunity.
Despite the tendency for the gland to shrink in size, antioxidants such as vitamin C, vitamin E, selenium, zinc and beta-carotene can help to prevent shrinkage and enhance cell-mediated immunity.
In the 1960’s research showed that immature white blood cells “incubate” in the thymus gland for a period of time. When they exit the gland they have been transformed into specific types of lymphocytes, such as helper T cells, suppressor T cells or cytotoxic T cells.
By the 1970’s medical research revealed that the thymus gland was similar to other hormone producing glands, such as the thyroid and pituitary. Scientists later discovered that the thymus gland secretes hormones. One of these is called thymosin. These hormones act at distant sites to influence the development and function of a variety of immune cells.
By the 1990’s researchers had discovered that at least four different hormones are secreted by the gland. These include the thymosins, a group of 40 or so related peptides called thymic fraction 5, thymopoiten, thymulin and thymus humoral factor. These hormones have been shown to have a broad range of action, well beyond simply maturing and differentiating T cells.
Thymus gland hormones can increase cytokines, including interleukin-2, interferon, colony stimulating factor and others. Thymus hormones can also cause greater numbers of T cells to develop more IL-2 receptors, which is important to create a rapid white blood cell proliferation against invading microorganisms. In addition, thymus hormones can increase disease-fighting antibodies.
Thymic hormones also prevent bone marrow injury and subsequent reduction in white blood cells that is frequently produced by chemotherapy and radiation treatments for cancer.
As the thymus gland shrinks with age, the blood levels of thymus hormones also declines. Scientists have shown a significant drop in thymosin levels between the ages of 20 and 40. Thymulin, a zinc activated hormone also drops in aging adults. This is not surprising, as the gland itself shrinks due to aging, stress, disease, radiation and poor nutrition.
There is an interesting synergistic relationship between thymus hormones and the hormones of the pituitary gland, especially growth hormone (GH). Thymus hormones increase the number and activity of T cells, which can secrete and release growth hormone and growth hormone releasing factor. There is also a relationship between thymus hormones and the thyroid gland. For these reasons, it is likely that restoring hormone levels as we age will favorably influence the thymus gland.
There is a well known and “normal” reduction in several hormones as we age, just as there is with thymus gland hormones. Doctors replace many hormones in aging patients, including thyroid hormone, adrenal hormones, such as DHEA and cortisol, insulin in diabetes, growth hormone, estrogen, progesterone and testosterone. However, physicians do not routinely replace thymus hormones.
There is a substantial body of scientific literature that shows that administering thymus hormone is beneficial to a variety of medical problems, including asthma, hay fever, allergies, chronic fatigue syndrome, rheumatoid arthritis, cancer, and hepatitis B and C. Studies have shown that thymus gland extracts are non-toxic and free of side effects. Although the FDA has not yet approved thymus extracts for the treatment of disease, doctors in Europe routinely use thymosins in the treatment of certain cancers, influenza and infectious diseases such as herpes.
Supplements that support thymus gland activity:
- Thymus extracts
- Thymic protein A
- Vitamin A
- Vitamin B6
- Vitamin E
- Beta carotene
- L-arginine
- Zinc
- Selenium
Lymph, Lymphatic Circulation and Lymph Nodes
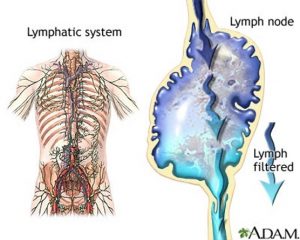 Lymph is a clear, watery liquid that begins as fluid flowing between cells. The fluid that surrounds cells is called interstitial fluid. Once interstitial fluid drains into the network of lymph capillaries it is called lymph. From lymphatic capillaries, lymph flows into larger vessels called lymphatics. The lymphatic circulation occurs in every part of the body from head to toe. Lymph nodes are found in many places along the lymphatic circulation, with higher concentrations in the neck, armpits, chest, abdomen and groin.
Lymph is a clear, watery liquid that begins as fluid flowing between cells. The fluid that surrounds cells is called interstitial fluid. Once interstitial fluid drains into the network of lymph capillaries it is called lymph. From lymphatic capillaries, lymph flows into larger vessels called lymphatics. The lymphatic circulation occurs in every part of the body from head to toe. Lymph nodes are found in many places along the lymphatic circulation, with higher concentrations in the neck, armpits, chest, abdomen and groin.
Lymph nodes are masses of lymph tissue covered by a fibrous capsule. They range in size up to 0.8 inches and they contain internal spaces where scavenging white blood cells, such as macrophages, ingest bacteria and other cellular debris. There are many lymph nodes along the lymphatic circulation before the lymph drains into the venous blood system in the chest.
When you notice a sore lymph gland in your neck during a sore throat or other viral infection, it means that there is a battle going on in the gland as your immune cells attack the invading virus. Lymph glands can also enlarge in other medical conditions such as metastatic cancer.
The lymphatic circulation is just as extensive as the blood circulation in your body. However, unlike the blood, which has a heart to pump it, there is no pump to move the lymph fluid except for the contraction of muscles in your body. When muscles contract, they compress the lymph pathways, thereby creating a pumping action. This is another important reason to engage in regular physical exercise. The more exercise, the better the lymph flow in your body. When people do not exercise, the lymph flow reduces and can create lymph stagnation, or stasis. Doctors believe that lymph stasis may be an important contributor to low oxygenation of tissues and the development of cancer.
One of the best ways to keep your lymph flowing is use of a mini-trampoline or rebounder. When you bounce on a trampoline, your body experiences changes in gravity that moves the lymph fluid. Some researchers believe that the rebounder is the single most beneficial form of exercise because of its widespread influence on lymph flow and immune function.
Apoptosis: Programmed Cell Death
Apoptosis is the process by which cells in the body commit suicide in response to problems within the cell or to signals from outside the cell. It is also called “programmed cell death”.
Apoptosis is an ingenious and essential aspect of your body wisdom. Apoptosis is wired into every cell of your body in order to prevent any cell from growing without regulation or regard for the over-all function of the body in general. It is especially important in preventing cancer cells from proliferating in your body. (See How cancer cells develop at the cellular level).
Normally cells divide for a certain number of times and then apoptosis kicks in and the cell dies. There are at least twelve tumor suppressor genes that create proteins that induce apoptosis when needed. P53 is a major tumor suppressor gene that must mutate in order for cancer to develop.
Apoptosis creates cell death by DNA cleavage, fragmentation of the cell nucleus and cell membrane disturbances that cause the cell to die, leading to phagocytosis by immune cells.
Apoptosis is one the remarkable regulatory systems in the body and is another example of the enormous wisdom built into our wondrous bodies.
Stem Cells
There are many types of stem cells. The best example occurs when a sperm fertilizes an ovum in the female uterus. The fertilized egg is a single cell that has the potential to form an entire human being. This form of stem cell is called totipotent, which means that it has unlimited ability to form new cells.
Stem cells are also found in children and adults and here they are called multipotent. The best example of a multipotent stem cell is the blood stem cell. Blood stem cells reside in your bone marrow and can even be found circulating in the blood stream. Blood stem cells perform the critical role of continually replenishing our supply of blood cells – red blood cells, white blood cells and platelets. And the do so throughout your life. You cannot survive without blood stem cells. They are also crucial in the regenerative process in your body.
As mentioned, stem cells are an essential part of your body and its ability to regenerate itself. Different classes of stem cells are found in umbilical blood and in the fetus. Using fetal stem cells in medical research and therapy is controversial and raises lots of ethical questions. Our government is considering this issue at the present time.
The applications of stem cell research are enormous. They can be used to regenerate tissues, as is the case of their use in Parkinson’s Disease where almost 100% recovery has been documented. They may be used to create human organs in the future and they offer an incredible anti-aging tool.
Stem cells are perhaps the most dramatic example of the creative intelligence that permeates your body. Imagine a single cell that has the knowledge and ability to produce a complete human being!
Your Mind: Thoughts, Emotions, Beliefs and Attitudes
I include the mind as a component of the immune system because aspects of consciousness play such a pivotal role in how immunity functions. In fact, most researchers in the mind-body field have concluded that they are one system, not two. Candace Pert has done extensive research on neurotransmitter function. She writes in her book, Molecules of Emotion, “Mind doesn’t dominate body, it becomes body – body and mind are one”. To review the unifying aspects of the bodymind, please refer to Your mind and immune system are intimately connected to each other.
The following states of mind or experiences have been shown in scientific research to weaken the immune system:
- Chronic stress
- Bereavement
- Divorce or separation
- Loneliness and social isolation
- Marital conflict
- Depression
- Anxiety
- Pessimism
- Lack of control
- Low self-esteem
- Feelings of hopelessness and helplessness
While the following states of mind or experiences have been shown in scientific research to strengthen the immune system:
- Relaxation
- Meditation
- Humor and laughter
- Social support and relationships
- Optimism
- Expressing emotions
- Increase your self-esteem
- Gain control in your life
- Commit to a challenging goal
- Belief, faith, and spirituality
Your health is your responsibility. Every cell in your body is fully committed to your well being. They function based on a creative intelligence as powerful and mysterious as life itself. You are part of that infinite power. Health is your birthright and disease is simply a lesson along the way to align you more closely to your true nature.

